Key takeaways
PTSD is a mental health condition triggered by experiencing or witnessing traumatic events.
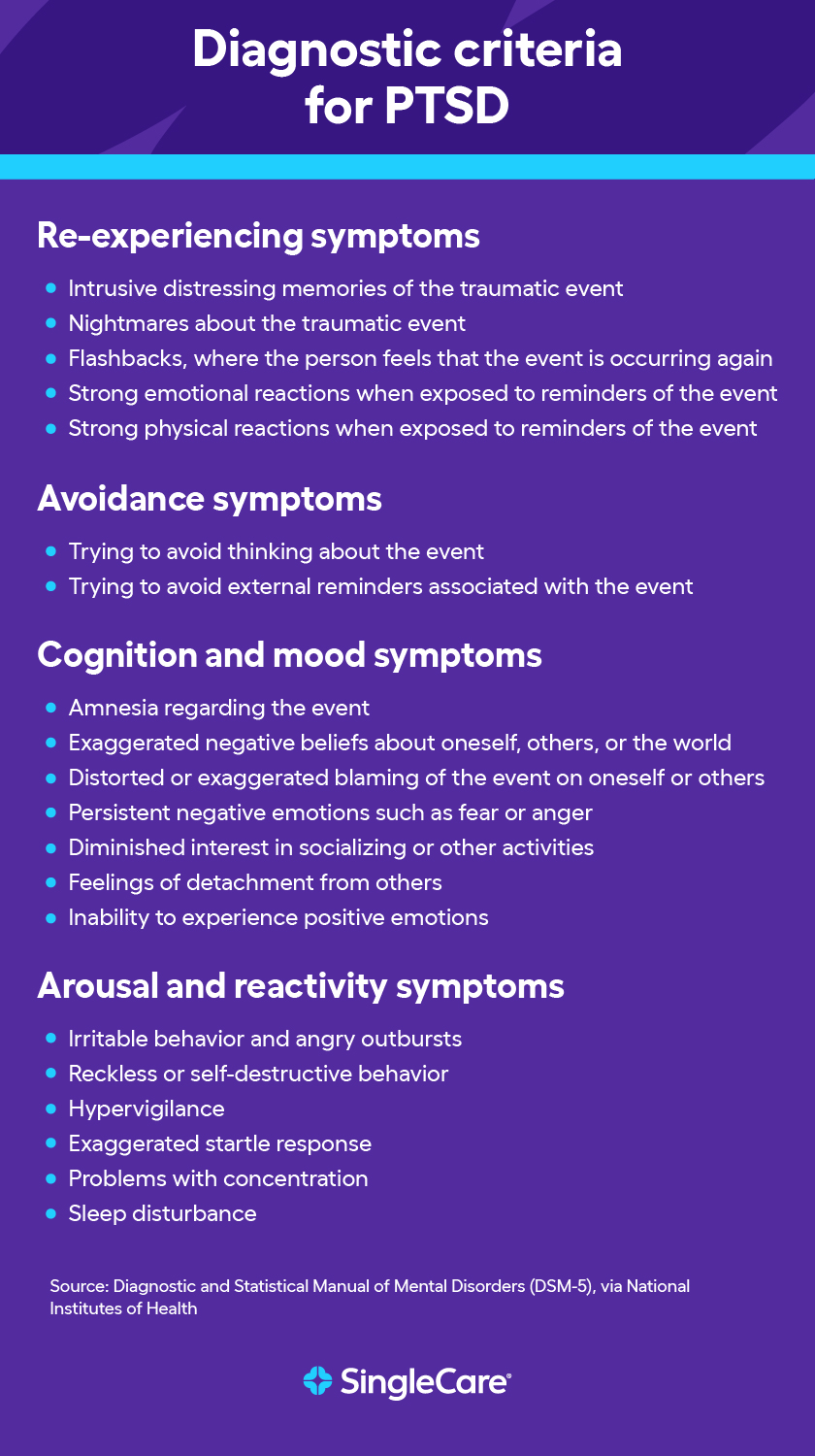
Symptoms may include flashbacks, anxiety, avoidance of triggers, negative thoughts, difficulty sleeping, nightmares, hypervigilance, exaggerated startle response, difficulty concentrating, irritability, or outbursts of anger. It can take months or even years for PTSD symptoms to emerge.
PTSD is considered a disabling condition by the Social Security Administration and the United States Department of Veterans Affairs. People with PTSD may be eligible for disability benefits.
About 5% of U.S. adults have PTSD in any year, according to the National Center for PTSD, and it affects 8% of adolescents aged 13 to 18, according to the American Psychiatric Association.
Treatment options for PTSD include cognitive therapies, medications like Zoloft or Paxil, and a healthy lifestyle such as eating well, exercising, getting quality sleep, maintaining personal relationships, and managing stress.
What is PTSD?
Post-traumatic stress disorder (PTSD) may occur in people who have experienced a frightening or unexpected event or even a series of events over time. PTSD causes upsetting and unwanted physical and emotional reactions. Although it is often associated with combat veterans, PTSD can happen to anyone.
Factors that make developing PTSD more likely include inherited mental health conditions, personality type, and biological factors. The symptoms vary drastically between different people. This guide will help PTSD patients and their families understand the disorder and learn what they can do to manage it.
What is a traumatic event?
A traumatic event poses a threat of serious injury or death, and that causes feelings of intense fear and helplessness after it happens. These events are stressful, frightening, distressing, difficult to cope with, or out of the person’s control. This causes intense emotional and physical reactions that may last long after the initial event. Such events include:
- Serious accidents
- Severe injury
- Sudden illness
- War and military combat
- Natural disasters
- Bullying
- Physical, verbal, or sexual abuse
- Death of a loved one
Differences between PTSD and C-PTSD
Generally, a single event causes PTSD, whereas long-term, chronic trauma causes complex post-traumatic stress disorder (C-PTSD). Long-term events include prolonged domestic violence, physical or sexual abuse as a child, and extreme situations such as slavery, torture, or genocide. Some experts have estimated that C-PTSD affects 1% to 8% of the global population.
Although both conditions lead to similar psychological and behavioral stress responses, people suffering from C-PTSD also experience trouble with emotion regulation, identity, sense of self, or forming and maintaining relationships.
Is PTSD a disability?
Yes, PTSD is considered a disabling condition by the Social Security Administration and the United States Department of Veterans Affairs. Those living with PTSD who have documented evidence of their condition may be eligible for disability benefits.
Social Security disability benefits
Receiving disability benefits is often a long process, even if a patient meets all the criteria. Eligible patients are sometimes even rejected the first time they apply. However, it is possible to receive benefits by reapplying with the proper documentation.
To receive Social Security disability benefits, someone living with PTSD must have documentation of the following:
- Exposure to actual or threatened death, serious injury, or violence
- Subsequent involuntary re-experiencing of the traumatic event (for example, intrusive memories, dreams, or flashbacks)
- Avoidance of external reminders of the event
- Disturbance in mood and behavior
- Increases in arousal and reactivity (e.g., exaggerated startle response, sleep disturbance)
In addition, the person must have one of the following:
- Extreme limitation of one or marked limitation of two of the following areas of mental functioning:
- Understanding, remembering, or applying information
- Interacting with others
- Concentrating, persisting, or maintaining pace
- Adapting or managing oneself
- The disorder is persistent. The person has a medically documented history going back at least two years that includes both treatment and therapy or support.
- The person must also have difficulty adjusting to changes in their daily life. This includes challenges in handling situations that come with regular activities, such as holding down a job.
For more detailed information on the eligibility criteria and the application process for Social Security disability benefits, visit the official website.
Veteran benefits
To receive VA benefits, someone living with PTSD must be a veteran of the armed forces and meet certain qualifications:
- The traumatic event happened during service
- The person can’t function as well as before due to PTSD symptoms
- A healthcare provider has diagnosed the person with PTSD
Traumatic events do not necessarily need to be combat-related. Any veteran who suffered a serious injury, experienced personal or sexual trauma or violation or was threatened with injury, sexual assault, or death during his or her service may be eligible.
The VA also runs the National Center for PTSD (founded in 1989), which provides millions of dollars annually to PTSD and traumatic stress research.
For more information on how to apply for VA benefits and learn about eligibility requirements, visit the official VA website.
PTSD in adults
What causes PTSD in adults?
Some common events that cause PTSD include:
- Serious accidents
- Physical or sexual assault
- Abuse
- Serious health problems
- Childbirth experiences, such as miscarriages
- Death of a close friend or family member
How common is PTSD in adults?
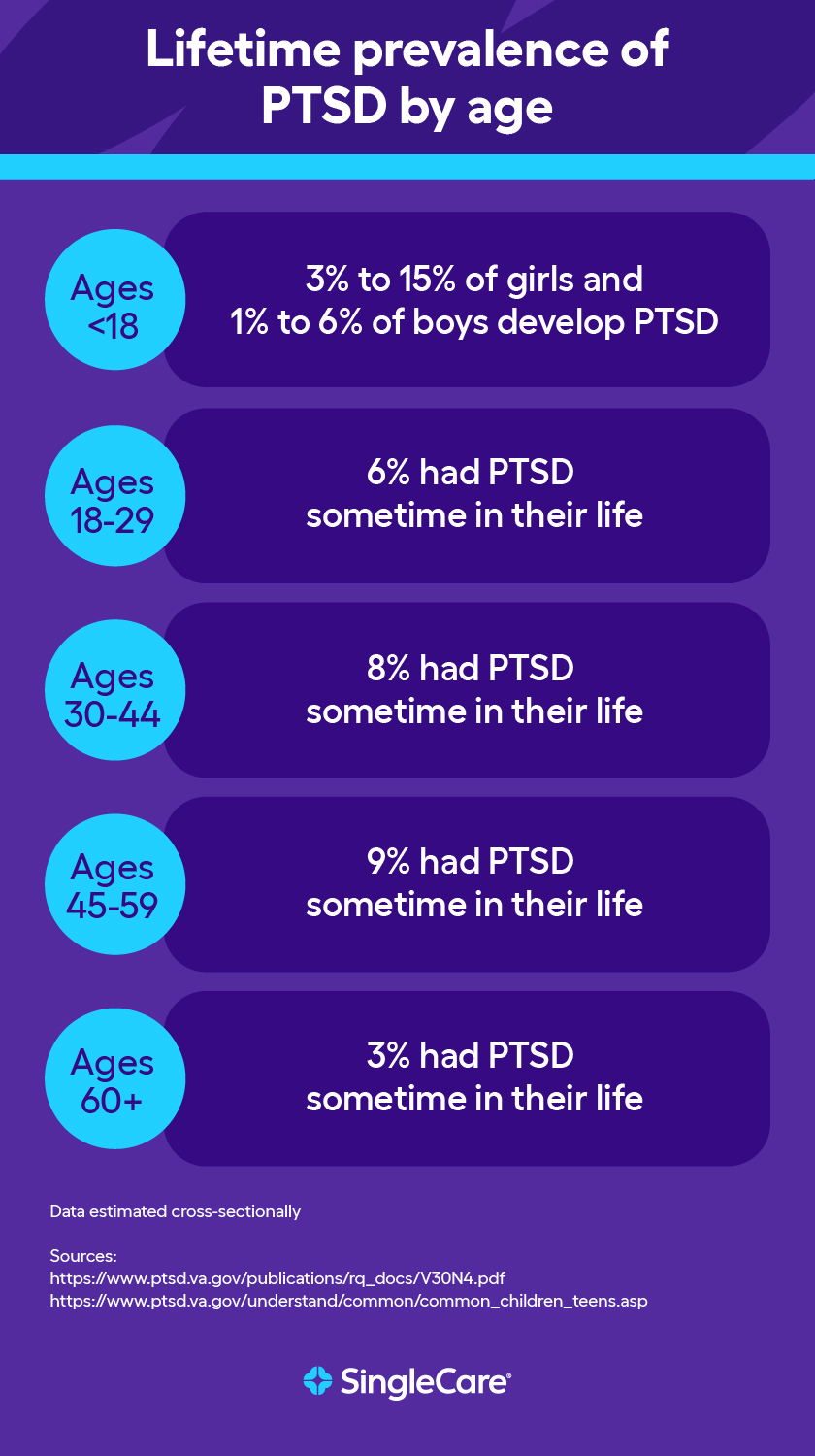
According to the National Center for PTSD, the majority of people who experience a traumatic event will not develop PTSD. About 5% of U.S. adults have PTSD in any year. In 2020, an estimated 13 million Americans experienced PTSD.
PTSD symptoms in adults
Symptoms of PTSD may emerge soon after the traumatic event or even years later. One study suggested that up to 25% of people experiencing PTSD had delayed-onset PTSD, where symptoms did not emerge until six months or more after the initial traumatic event. People with PTSD may also try to hide their symptoms from close friends and family and may not share that they’ve suffered a traumatic event. Some common symptoms in adults include the following:
- Re-experiencing: Re-experiencing involves reliving a traumatic event vividly and involuntarily. Those with PTSD react differently to re-experiencing, with up to 70% showing an elevated heart rate and the other 30% dissociating and showing no response.
- Avoidance: To protect themselves, those with PTSD will try to avoid any situation that reminds them of a traumatic event. In one study, 43% of subjects with PTSD showed symptoms of avoidance.
- Increased negative thoughts and feelings: Those with PTSD might begin to have negative thoughts about themselves or other people. This may manifest in various ways, with several negative thinking patterns.
- Hyperarousal (reactivity): In one study, 97.3% of adult patients with PTSD had arousal symptoms such as difficulty sleeping, hypervigilance, exaggerated startle response, difficulty concentrating, and irritability or outbursts of anger.
The impact of PTSD on adults
PTSD affects individuals in multiple ways, including their mental, physical, social, and work life, as well as their long-term health. People with PTSD may also struggle with interpersonal problems, parenting difficulties, and household income.
PTSD may increase the risk of developing health problems due to sleep disturbances, physical symptoms, obesity, depression, and substance abuse. It is also strongly associated with suicidal behavior. In fact, 80% to 90% of those with PTSD experience at least one other mental disorder during their lifetime.
These comorbidities may make it difficult for those with PTSD to maintain a stable job and may increase their healthcare costs due to them needing medical treatments or drugs to manage either disorder. There are indirect costs, including unemployment, loss of productivity, and premature mortality. One study estimated that the direct and indirect costs of PTSD amounted to $19,630 per individual per year in 2018.
PTSD in children
Although the focus is often on adults, PTSD may occur in anyone at any age. It affects 8% of adolescents aged 13 to 18.
What causes PTSD in children?
An event that caused someone in their lives to be seriously injured or killed could cause children to develop PTSD, such as in:
- Natural or manmade disasters, like floods or house fires
- Serious accidents, such as car accidents
- Terrorist attacks
- War/combat
- Rape, sexual assault, or intimate partner violence
- Severe bullying
- Illness or death of a family member or close friend
The likelihood of children developing PTSD after one of the above events depends on the severity of the trauma, how their parents reacted, and how close the child was to the trauma. This closeness could be physical (such as witnessing a violent crime) or emotional (such as losing a close friend or family member). Direct exposure means a child has experienced trauma firsthand or witnessed it happen to someone else. Learning about the death of a close friend may indirectly expose children to trauma.
How common is PTSD in children?
The National Center for PTSD cites previous studies that have shown that 15% to 43% of girls and 14% to 43% of boys experience at least one traumatic event in their life. Of these, 3% to 15% of girls and 1% to 6% of boys will develop PTSD, with specific rates depending on the type of trauma.
PTSD symptoms in children
Children experiencing PTSD display a variety of symptoms according to the nature of the trauma. Many of the symptoms are similar to those adults experience:
- Reliving the event
- Nightmares and other sleep disturbances
- Becoming upset when something causes memories of the event
- Intense, ongoing fear or sadness
- Irritability
- Constantly being on the lookout for possible threats
- Denying that the event happened or feeling numb
- Avoiding places or people associated with the traumatic event
The impact of PTSD on children
The impacts of PTSD on children go well beyond childhood and may follow children into adulthood if left unaddressed. Some common effects include lower grades, more suspensions and expulsions, and increased interactions with the juvenile justice system.
PTSD may also affect a child’s neurodevelopment, which may change their long-term response to other stressors, making them more likely to develop psychiatric disorders. It may even make it difficult for them to regulate, identify, and express emotions or relate to others.
PTSD can negatively impact a child’s physical health, too. Studies have found a link between trauma and increased reports of physical health issues, including chronic conditions like heart disease and cancer, especially in survivors of childhood abuse and neglect. Trauma survivors also tend to use medical services more frequently, leading to higher healthcare costs.
Who’s most likely to develop PTSD?
Anyone likely to experience traumatic events is more likely to develop PTSD.
The disorder itself was first identified as a result of diagnoses of Vietnam War combat veterans. In combat, it’s possible to experience many of the risk factors listed above (dangerous events, getting hurt, seeing another person get hurt, extreme fear) all in a single day or even within a few minutes.
As PTSD research became more prevalent, medical professionals began to understand that noncombat traumatic events could also trigger the disorder.
A research study identified occupations that are high risk for PTSD. These were:
- Police officers
- Firefighters
- Ambulance personnel
- Healthcare professionals
- War correspondents
- Employees at retail establishments at high risk of armed robbery
Women are more likely to be diagnosed with PTSD than men, and it may have to do with the nature of the trauma that women experience.
How long does PTSD last?
PTSD can last for years without proper treatment, but the duration varies depending on the person and the approach to care. While PTSD was once thought to be a chronic condition, newer treatments—especially trauma-focused therapies—are designed to address the root causes of the disorder.
One innovative method being studied is massed treatment, where therapy that typically spans six weeks is condensed into just five days. Research shows that this intensive approach can be just as effective, or even more effective, than traditional therapy formats, offering some individuals a quicker path to recovery.
Treatment options for PTSD
It is important to find a licensed healthcare provider for an evaluation.
Adults
The American Psychological Association (APA) recommends four first-line treatment options:
- Cognitive Behavioral Therapy (CBT)
- Cognitive Processing Therapy (CPT)
- Cognitive Therapy
- Prolonged Exposure
It also conditionally recommends another four treatment options. There is evidence that these also provide positive outcomes for patients, but they might be less applicable to certain subgroups of people with PTSD:
- Brief Eclectic Psychotherapy
- Eye Movement Desensitization and Reprocessing (EMDR) Therapy
- Narrative Exposure Therapy (NET)
- Medications
The APA has conditionally recommended four medications for treating PTSD:
Children and adolescents
Children who have PTSD may be reluctant to talk about the event that caused their trauma. Therefore, finding a psychotherapist experienced in talking to children and adolescents is important. Cognitive-behavioral therapy (CBT) may also help children change their thought patterns and feelings by altering their behavior to reduce their fears. One study reported that 92% of children no longer met the diagnostic criteria for PTSD after CBT.
A psychiatrist may also prescribe medication to help manage symptoms as part of the treatment. The following medications are commonly used to help manage PTSD symptoms in children and adolescents:
Lifestyle changes for PTSD management
Treating PTSD may require lifestyle changes to reduce symptoms and improve your quality of life. Some common changes include giving up alcohol and drugs and prioritizing exercise, a healthy diet, volunteer work, personal relationships, sleep, and stress management.
It might be necessary to move if you live in an area that makes you feel unsafe, especially if you live where the traumatic event occurred. Moving may make it easier to feel safe in your home and community. Just be mindful that moving itself is often stressful. Take steps to make the move easier, including asking for help and planning the move. Also, note that you should not consider moving as a substitute for professional help.
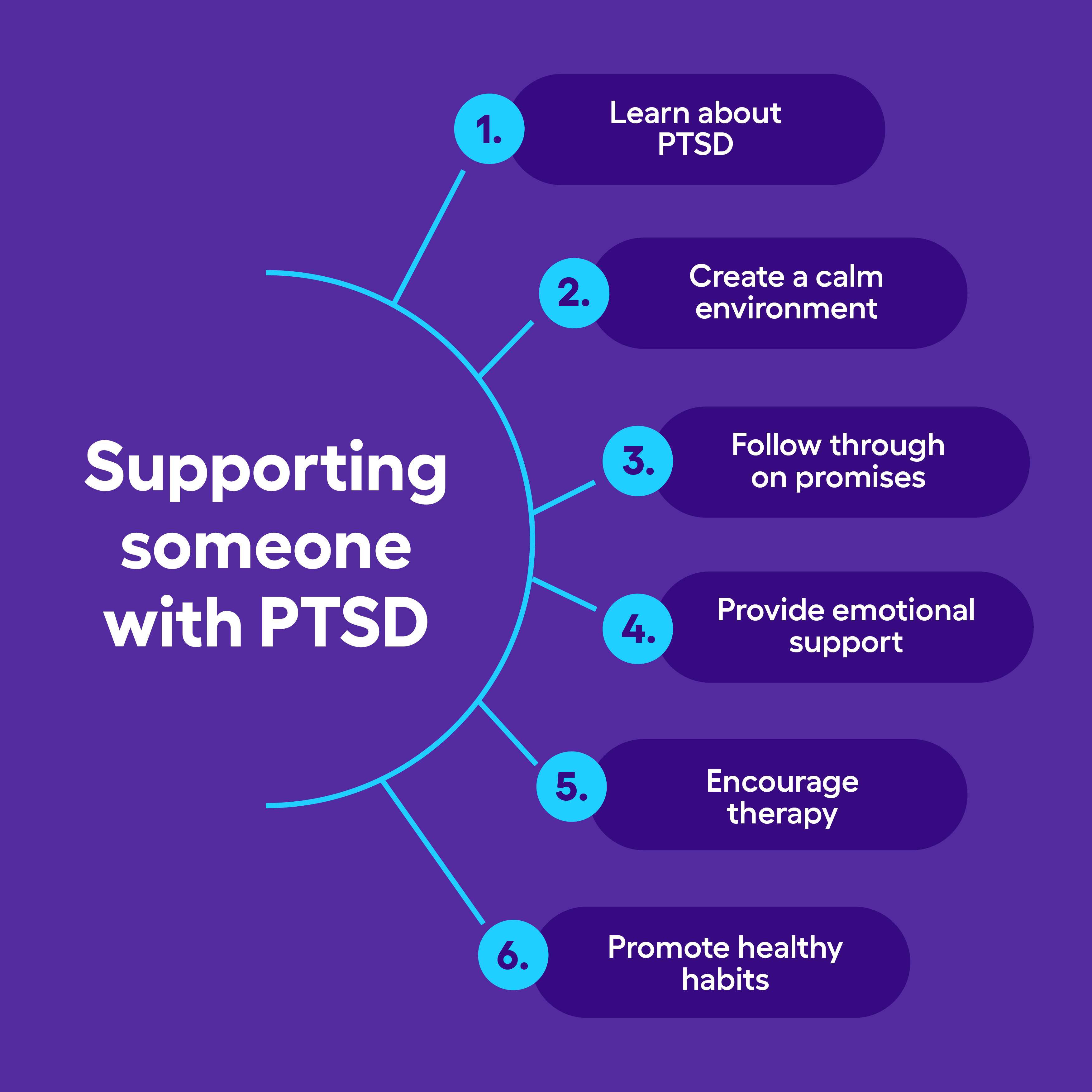
Supporting someone with PTSD
When someone you care about has PTSD, it not only changes that person’s life, but it may also affect your life in unforeseen ways. For example, a person with PTSD may begin acting differently or anger easily and may withdraw and stop wanting to do things together.
This will probably confuse you at first and may even cause you to feel scared and angry. Just remember that these reactions are common for people with PTSD. You can take steps to make things easier for your loved one.
Offer support
If you want to offer your support to someone with PTSD, some things to do include:
- Educate yourself on PTSD symptoms, triggers, and coping strategies.
- Minimize stress at home by ensuring the person has space and time for rest.
- Speak of the future and make plans to help the person overcome feelings that their future is limited.
- Follow through with your promises.
- Provide emotional support by being present, listening, reassuring, and affirming their strengths.
- Offer to provide transportation to therapy or even to participate in a support group with them if they’re open to it.
- Promote a healthy lifestyle by inviting them to exercise (like walking together) or bringing a nutritious meal.
- Remind them what they enjoy and help them reconnect with their hobbies and interests.
Remember that offering support may take a toll on you as well, affecting your health and possibly even causing you to become sick or depressed. Don’t feel guilty; remind yourself that it’s normal to feel bad if things progress very slowly. Take some time for yourself if you need to. It’ll be more challenging to take care of your loved one if you also have health issues to deal with.
Things to avoid
Remember that your loved one may not want your help. This is common in those affected by PTSD.
- Don’t force things. Ensure your loved one knows you’re there if they need help, and try to give the person space.
- Avoid triggers. Triggers may be places, people, or situations that remind your loved one of the event that caused their PTSD.
- Don’t rush recovery. Avoid pressuring your loved one to talk about their trauma and respect their boundaries.
Using technology to manage PTSD
Telemedicine technologies like clinical video teleconferencing (CVT) and web-based interventions can provide mental health services to those with PTSD. Many mental health apps are also available, including mood and symptom trackers, journals and gratitude apps, guided meditation apps, positive distraction apps, and sleep apps. Some wearable devices can help people with PTSD monitor symptoms and provide detailed information to their healthcare provider, such as heart rate, sleep quality, and stress levels.
Get help with PTSD now
There are a variety of resources available if you or a loved one is experiencing PTSD, even if you haven’t received a formal diagnosis.
Organizations
- The U.S. Department of Veterans Affairs operates the National Center for PTSD. Its website contains a wealth of information for those who have PTSD, especially combat veterans.
- Anxiety & Depression Association of America is a nonprofit organization dedicated to the prevention, treatment, and cure of PTSD and other disorders.
- National Alliance on Mental Illness is a mental health organization whose mission is to improve the lives of Americans affected by mental illness.
Support groups and hotlines
- The U.S. Department of Veterans Affairs hosts a page with peer support groups
- Anxiety & Depression Association of America Support Groups
- Local trauma and PTSD support groups
- SAMHSA’s National Helpline is an information service for those facing mental disorders, including PTSD: 1-800-662-HELP (4357)
- CPTSD (Complex PTSD), Cleveland Clinic (2023)
- Disability, Social Security Administration
- Disability compensation for PTSD, U.S. Department of Veteran Affairs (2024)
- Post-traumatic stress disorder (PTSD), Substance Abuse and Mental Health Services Administration (2023)
- Causes – Post-traumatic stress disorder, National Health Service (2023)
- How common is PTSD in adults?, U.S. Department of Veteran Affairs
- Post-traumatic stress disorder: a state-of-the-art review of evidence and challenges, World Psychiatry (2019)
- Reexperiencing/hyperaroused and dissociative states in posttraumatic stress disorder, Psychiatric Times (2008)
- Avoidance symptoms and assessment of posttraumatic stress disorder in Arab immigrant women, Journal of Traumatic Stress (2008)
- Changing negative thinking patterns, National Center for PTSD (2013)
- Diagnosis and management of post-traumatic stress disorder, American Family Physician, (2003)
- Posttraumatic stress disorder in adults: Impact, comorbidity, risk factors, and treatment, The Canadian Journal of Psychiatry (2014)
- Posttraumatic stress disorder in the National Comorbidity Survey, Archives Of General Psychiatry (1995)
- The economic burden of posttraumatic stress disorder in the United States from a societal perspective, Journal of Clinical Psychiatry (2022)
- What is posttraumatic stress disorder (PTSD)? American Psychiatric Association (2022)
- Post-Traumatic Stress Disorder, Cincinnati Children’s (2022)
- How common is PTSD in children and teens?, U.S. Department of Veteran Affairs
- Understanding child trauma, Substance Abuse and Mental Health Services Administration (2024)
- PTSD and physical health, U.S. Department of Veteran Affairs
- Occupational risk for post-traumatic stress disorder and trauma-related depression: A systematic review with meta-analysis, International Journal of Environmental Research and Public Health (2020)
- Research on Women, Trauma, and PTSD, U.S. Department of Veteran Affairs
- PTSD treatments, American Psychological Association (2020)
- Cognitive-behavioral therapy for PTSD in children and adolescents: A preliminary randomized controlled trial, American Academy of Child and Adolescent Psychiatry (2007)
- Reduce PTSD symptoms through lifestyle changes, Valley Oaks Health Hub (2019)
- The National Center for PTSD
- Anxiety & Depression Association of America
- National Alliance on Mental Illness
- Peer support groups, U.S. Department of Veteran Affairs
- Support groups, Anxiety and Depression Association of America
- Find a trauma and PTSD support group, Psychology Today