Stay-at-home orders, social distancing, and other preventive measures forced many in-person activities to be quickly adapted for virtual platforms. Zoom and other video conferencing tools hosted work meetings, school lessons, and holiday celebrations. Even health visits were moved online or over the phone for people with non-emergency symptoms and illnesses. Telehealth is not a new concept, but its adoption was accelerated quickly over the past year. To better understand how Americans are adapting to virtual health visits, SingleCare conducted a telehealth survey of 1,700 adults in January 2021.
RELATED: What is telehealth?
Key findings:
- 43% of respondents don’t know if telehealth services were offered by their healthcare providers pre-pandemic.
- Telehealth services are offered to at least 58% of respondents by their healthcare providers.
- 74% of respondents are open to using telehealth services.
- Two-thirds of respondents are willing to use telehealth services for common illnesses and follow-up visits.
- Saving time, not having to travel, and appointment availability are the most appealing aspects of telehealth.
- Diagnosis errors, exam challenges, and quality of care are the most common concerns of telehealth.
- 68% of respondents would prefer in-person visits over telehealth visits after the pandemic.
- Only 5% of respondents had used a telehealth service prior to the pandemic (2019 or earlier).
- Of those who have used telehealth services, 78% were satisfied with their experience.
- Insurance or Medicare completely covered telehealth services for 60% of respondents.
- 62% of respondents pay an average of $0 to $30 per telehealth visit.
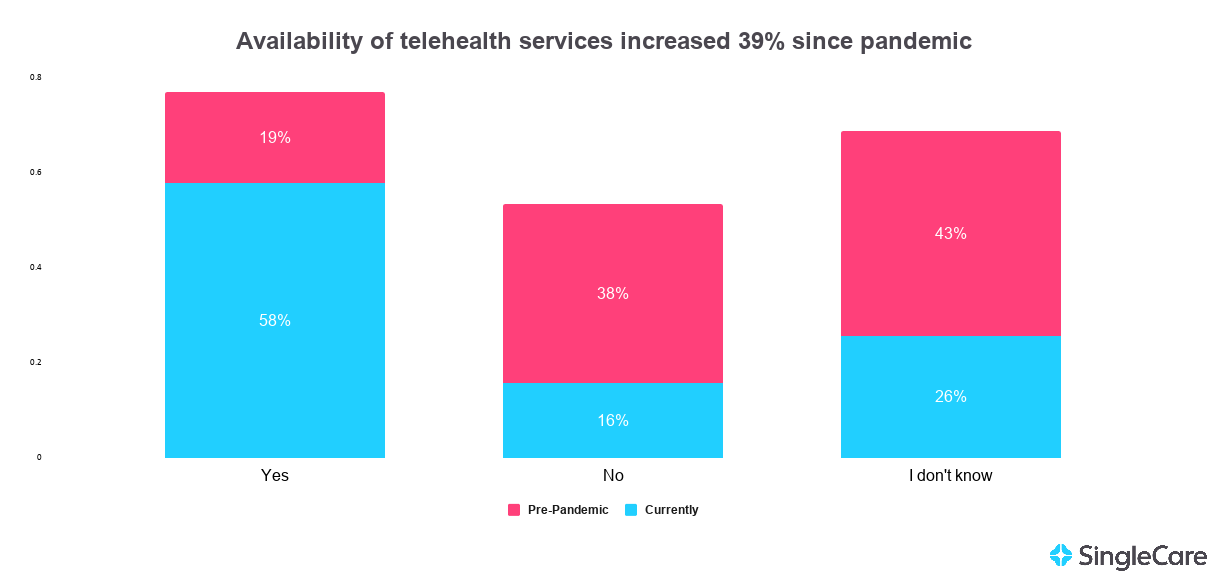
43% of respondents don’t know if telehealth services were offered by their healthcare providers pre-pandemic
Before the coronavirus outbreak, 43% of respondents reportedly did not know if their healthcare provider offered telehealth services. Less than 1 in 5 respondents reported that telehealth services were available to them.
- 19% Yes, telehealth services were available pre-pandemic
- 43% I don’t know if telehealth services were available pre-pandemic
- 38% No, telehealth services were unavailable pre-pandemic
Telehealth services are now offered to at least 58% of respondents by their healthcare providers
Today, only 16% of respondents reported that their healthcare provider does not offer telehealth services. The reported number of providers offering telehealth services also increased from at least 19% to 58% during the pandemic, according to our survey.
- 58% Yes, my provider currently offers telehealth services
- 26% I don’t know if my provider currently offers telehealth services
- 16% No, my provider does not currently offer telehealth services
74% of respondents are open to using telehealth services
Half of our survey takers (55%) have not used telehealth yet, but 74% of all respondents are willing to do so.
- 40% Yes, I have used telehealth services in the past
- 34% Yes, I have not used telehealth services, but I would consider it in the future
- 21% No, I have not used telehealth services in the past and would not consider it in the future
- 5% No, I have used telehealth services in the past and would not do so again
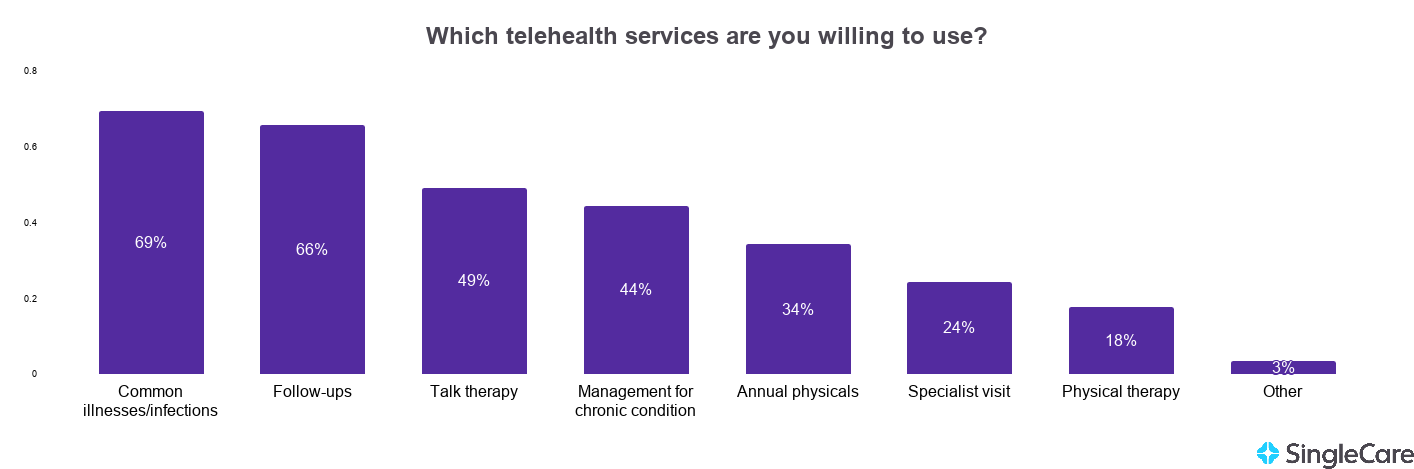
Two-thirds of respondents are willing to use telehealth services for common illnesses and follow-up visits
The majority of survey respondents were reportedly willing to use telehealth for common illnesses and infections as well as follow-up visits. They were less keen on using telehealth for annual physicals, specialist visits, and physical therapy.
- 69% Common illnesses/infections (cold, flu, sinusitis, allergies)
- 66% Follow-up visits (i.e., follow-up after a procedure or hospitalization)
- 49% Talk therapy
- 44% Management for a chronic condition (heart disease, diabetes, etc.)
- 34% Annual physical exams
- 24% Specialist visit (endocrinologist, OB-GYN, nutritionist, dermatologist)
- 18% Physical therapy
- 3% Other (i.e., prescription requests and refills, general medical questions, minor cuts/scrapes/reactions)
We talked to healthcare professionals to get their perspectives on using telehealth for this type of care.
There are mixed perspectives on whether annual physicals can be done via telehealth. Sachin Gupta, MD, a pulmonologist in the San Francisco Bay area says physical exams (including breast exams, Pap smears, and prostate exams) are not possible. On the other hand, Jenna Liphart Rhoads, RN, a nurse and educator for NurseTogether says it’s absolutely possible. Both mentioned that having thermometers, blood pressure monitors, oxygen sensors, and scales at home is helpful for these types of virtual visits.
“For those who have chronic health conditions (i.e. hypertension, diabetes, heart disease), virtual visits may not be practical because things such as blood pressure, blood sugar, and vascular wellness may not be able to be accurately measured virtually,” Rhoads says. “Someone with multiple chronic illnesses or symptoms that have exponentially increased would most likely need to be seen in-person for the most accurate diagnoses.”
“Physical therapy can absolutely be done through telehealth, especially when dealing with joint pains or a chronic injury,” says Alyssa Kuhn, DPT, a mobile therapist in Sandy, Utah. “In certain situations, I have found it to be better than in-person therapy because you understand how to actually complete the movements and mobility exercises at your own home.”
Many of the healthcare professionals we talked to encourage patients to view telehealth as a convenient starting point rather than an extra step or a hassle.
RELATED: How to find a therapist during a pandemic
Saving time, not having to travel, and appointment availability are the most appealing aspects of telehealth
A 2017 study found that the average time spent on an in-person visit was 121 minutes. This included time spent traveling, waiting, and actually seeing the doctor. Because telehealth does not require transportation, there was a 31% reduction in time needed for a telehealth visit by eliminating travel time alone. The amount of time saved with telehealth services versus office visits was the most appealing aspect of telehealth according to our survey takers.
- 74% Saves time
- 70% I don’t have to travel
- 53% Appointment availability
- 50% Ease of communication (i.e., myChart services, online prescription requests, online lab requests)
- 49% Online scheduling capabilities
- 44% Saves money
- 39% I feel more comfortable in my own home than a doctor’s office
- 2% Other (I don’t have to worry about getting COVID-19 from a doctor’s office)
Diagnosis errors, exam challenges, and quality of care are the most common concerns of telehealth
- 39% Errors in diagnosis
- 36% Exam challenges
- 31% Quality of care
- 39% If the doctor cannot diagnose me via telehealth, they’ll refer me for an in-person visit anyway
- 26% I have no concerns about telehealth services
- 22% Losing a feeling of connection with my healthcare provider
- 16% Privacy or security concerns
- 14% I’m not sure if telehealth services are covered by my insurance or Medicare plan
- 12% Difficulty in using technology
- 6% Physician burnout
- 5% Telehealth services are not covered by my insurance or Medicare plan
- 1% Other (poor internet connection, I don’t have a webcam, all of the above, I don’t understand telehealth, I have to see a doctor in-person for my condition, etc.)
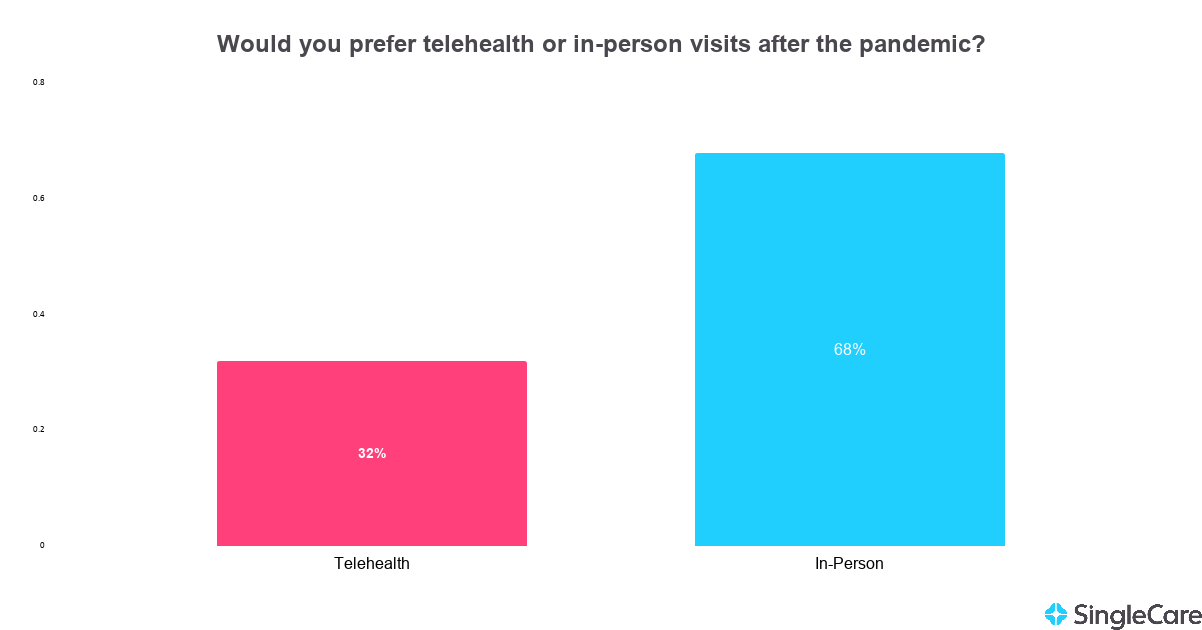
68% of respondents would prefer in-person visits over telehealth visits after the pandemic
More than two-thirds of our respondents said they would prefer in-person office visits over telehealth visits after the pandemic. This is in stark contrast to other telehealth surveys that were conducted in the year leading up to the coronavirus pandemic.
One survey in January 2019 found that 82% would definitely recommend virtual video visits to others, and 69% rated their virtual visit a 9 or 10 out 10 (10 being the best visit). Another survey conducted in July 2019 found that 81% of respondents were more likely to choose a provider who offered telemedicine services over one who does not.
Now, after a year of virtual visits, it seems as if some people are having second thoughts on telehealth. Our survey found that the majority would prefer in-person visits over telehealth after the pandemic is over.
RELATED: Why are Americans skipping healthcare services?
Only 5% of respondents had used a telehealth service prior to the pandemic
Stay-at-home orders and other preventive measures during the COVID-19 pandemic have accelerated telehealth adoption. We asked respondents about when they used telehealth services for the first time. Only 5% had reported using telehealth before the COVID-19 pandemic (2019 or earlier); whereas, 46% have used telehealth within the past year (2020).
- 7% Within the last month
- 21% Within the last six months
- 18% Within the past year
- 5% It’s been more than a year ago (2019 or earlier)
- 49% I have not had a telehealth appointment
Of those who have used telehealth services, 78% were satisfied with their experience
Although 26% of respondents were reportedly unwilling to use telehealth services and 68% would prefer in-person visits post-pandemic, 94% of respondents who have used telehealth services felt reportedly satisfied or neutral with their experience.
- 42% Extremely satisfied
- These respondents often mentioned that telehealth saves them time, it’s very easy, and they liked that they didn’t have to travel.
- 36% Somewhat satisfied
- These respondents reported that their experience was okay. The appointment was effective but it felt less personal than an in-person visit.
- 16% Neutral
- These respondents said that their goal was to ask their doctor questions or request a prescription rather than receive a diagnosis. Many of them said they prefer in-person visits.
- 4% Not satisfied
- These respondents questioned the quality of care they received or reported technology issues.
- 2% Extremely dissatisfied
- Several of these respondents reported that they never got to talk to their primary healthcare provider, but rather a nurse or a physician’s assistant.
Insurance or Medicare completely covered telehealth services for 60% of respondents
The Coronavirus Aid, Relief, and Economic Security Act (CARES Act), which was signed into law on March 27, 2020, paved the way for the widespread use of telehealth. This is evident from the 60% of survey respondents who reported that private insurance or Medicare completely covered their telehealth services.
- 60% Private insurance or Medicare completely covers my telehealth services
- 26% Private insurance or Medicare partially covers my telehealth services
- 8% I pay out of pocket for all of my telehealth services
- 6% Other (VA, Medicaid, etc.)
62% of respondents pay an average of $0 to $30 per telehealth visit
A 2017 Health Affairs study found that the average cost was $79 for a telehealth visit, $146 for an office visit, and $1,734 for an emergency visit for the most commonly treated conditions. The study also accounted for the cost of travel time for an in-person visit ($13 on average). Today, telehealth and office visits are closer in cost. In the adoption of the CARES Act, many private insurers charged the same rate for telehealth visits as in-person visits.
| Average out-of-pocket cost per visit | ||
|---|---|---|
| Telehealth | In-person | |
| $0 | 38% | 31% |
| $1-$20 | 12% | 14% |
| $21-$30 | 12% | 14% |
| $31-$40 | 6% | 7% |
| $41-$50 | 6% | 6% |
| $51-$60 | 2% | 2% |
| $61-$70 | 2% | 2% |
| $71-$80 | 6% | 6% |
| $81-$90 | 2% | 3% |
| $91-$100 | 3% | 4% |
| $101 or more | 11% | 11% |
As of October 2020, some private insurance providers (such as UnitedHealthcare and Anthem BlueCross BlueShield) started pulling back on telehealth coverage. You can find updated information on telehealth coverage on medicare.gov or medicaid.gov, or contact your insurance provider. Your doctor’s office may also be able to look up your coverage and copay estimates before your visit.
Our methodology
SingleCare conducted this telehealth survey online through AYTM on Jan. 29, 2021. This survey includes 1,700 United States residents adults ages 18+. Age and gender were census-balanced to match the U.S. population in age, gender, and U.S. region.