Key takeaways
Eating a balanced diet during pregnancy ensures that both the mother and the baby receive the essential nutrients they need.
The best pregnancy diet includes a variety of macro- and micronutrients, emphasizing fresh fruits, vegetables, whole grains, nuts, legumes, and fish.
The Mediterranean diet is highly recommended for pregnant women due to its balance of anti-inflammatory foods, monounsaturated fats, and plant-based omega-3s.
It is important to avoid alcohol, high mercury fish, unpasteurized dairy products, raw and undercooked meat and seafood, and to limit caffeine intake during pregnancy.
Through each of the three pregnancy trimesters, your baby continually grows. At the same time, many hormonal and physical changes occur in the mother’s body to accommodate the growing fetus. Eating a balanced diet is an essential part of ensuring that both mother and baby receive the nutrients they need.
“The vital nutrients from healthy foods ensure a healthy and more comfortable pregnancy journey. Healthy food lowers your risk of developing pregnancy-related complications that may harm you or the infant,” says Daniel Boyer, MD, a researcher at the Farr Institute. “Healthy nutrition is important for successful fetal development and reducing pregnancy-related symptoms like anemia, nausea, and morning sickness.”
Studies on the early metabolic programming of health and diseases suggest that healthy eating during pregnancy reduces the risk of chronic health diseases for the fetus, such as hypertension and Type 2 diabetes, through adulthood. If you’re wondering what foods are best in a pregnancy diet, keep reading to learn everything you need to know about healthy nutrition in pregnancy.
What’s the best pregnancy diet plan?
Many people erroneously believe that during pregnancy you should eat for two. That’s incorrect; you should focus on eating healthy, not more. “One could argue that a breastfeeding woman is eating for two, but a pregnant woman is definitely not,” says Dana Ellis Hunnes, Ph.D., a senior registered dietitian and assistant professor at UCLA Fielding School of Public Health, author of Recipe for Survival. “In the first trimester, you don’t need additional calories, and in the second and third trimesters, you will only need 200 to 500 extra calories per day.” That’s nowhere near double the recommended amount. If you did eat “for two” with twice the number of calories, you may gain an excessive amount of weight for both you and the fetus, which may make childbirth more difficult and lead to difficulty losing the weight postpartum.
Instead, the best pregnancy diet is balanced with macro- and micronutrients your body needs to foster a healthy pregnancy for mom and baby. Such diets include fresh fruits, leafy vegetables, legumes, whole grains, nuts, and fish—with less processed foods and fatty red meats.
A healthy diet decreases the chance of pregnancy complications, including gestational diabetes, hypertension, maternal obesity-related issues, preeclampsia, and preterm birth. Poor nutrition may limit your baby’s growth and can even lead to birth defects. Excess intake of sugar and fat can cause your baby to be larger than normal. Put simply, your pregnancy diet plan should bridge the gap between undernutrition and overnutrition. This common diet can help you get the balanced nutrition you need.
Mediterranean diet
The Mediterranean diet is an excellent choice for pregnant women. “A primarily plant-based diet, such as the Mediterranean diet, is a near-perfect diet for pregnancy,” says Hunnes. “It is filled with anti-inflammatory foods, high in monounsaturated fats, plant-based omega-3s, and vitamins and minerals naturally occurring in foods.”
This specific diet supplies the key nutrients that help with your baby’s growth and may decrease pregnancy complications such as gestational diabetes mellitus, urinary tract infections, emergency cesarean section, premature birth, and low birth weight. The Mediterranean diet was also associated with better sleep quality for pregnant mothers.
Moreover, the research indicates that a Mediterranean diet promotes a healthy birth weight, enhances growth for your baby, and reduces behavioral problems in childhood. A study referenced in the same systematic review reports that children of mothers who followed the Mediterranean diet in pregnancy had reduced hospital visits up to 2 years of age. 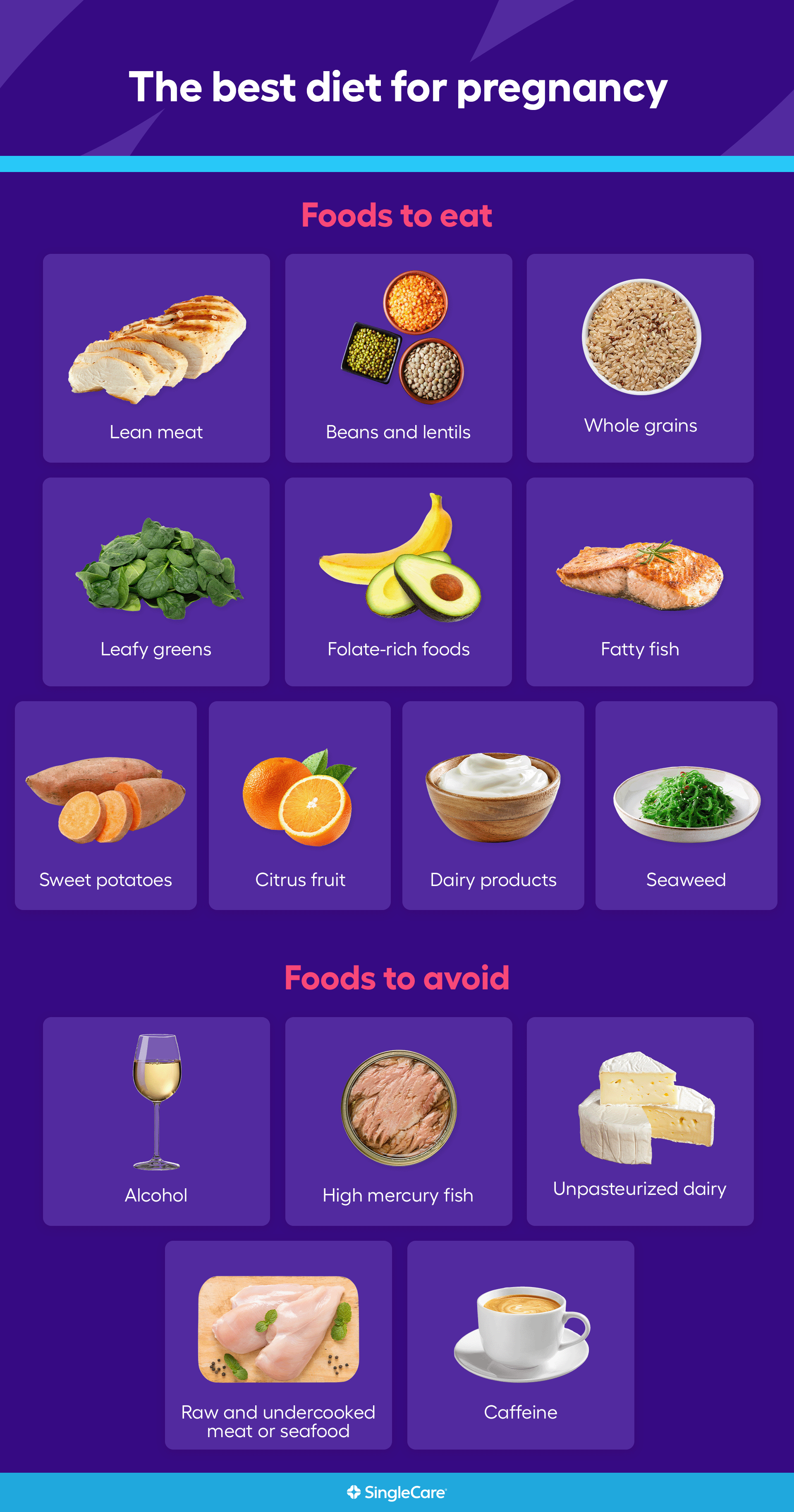
10 best foods for pregnancy
The best pregnancy diet includes a variety of food groups “like whole grains, fruits, nuts, seeds (high in omega-3 plant-sourced fats) and legumes,” says Hunnes. “It’s a diet filled with color from naturally occurring food sources, think red/orange bell peppers, leafy greens, blueberries, zucchini, walnuts and chia seeds.”
However, diet plans may differ based on eating customs, individual preferences, pregnancy cravings, budget, and chronic health conditions like diabetes and hypertension. In spite of that, a healthy pregnancy meal plan includes food choices that prioritize optimal health for mom and baby. A registered dietitian can help recommend meal plans tailored to your needs. Some great food choices to add to your meal plan are:
1. Lean meat
Protein supports the growth of the fetus. Lean meats, such as chicken and turkey, are excellent sources of protein because they provide complete amino acids, vitamin B12, iron, and zinc. If you are vegetarian or develop an aversion to meat during pregnancy, incorporate plant-based protein such as chickpeas, tofu, beans, lentils, whole grains, and high-protein vegetables like broccoli, asparagus, and Brussels sprouts.
2. Beans and lentils
The American College of Obstetricians and Gynecologists (ACOG) recommends beans and lentils as sources of iron for pregnant women. Iron is an essential micronutrient that makes the hemoglobin component of red blood cells. Pregnant women’s requirements increase during pregnancy from 18 micrograms to 27 micrograms daily. Red blood cells transport oxygen to your baby to help with immune function, brain, and other organ development. Studies indicate that fetal brain uses 60% of oxygen and needs three to four times more supply than an adult’s brain, which requires only 20% oxygen.
Studies show that iron is the most commonly deficient nutrient. If you’re having a hard time eating enough iron-rich foods, taking iron supplements during pregnancy can help.
3. Whole grains
Add whole grains like oats, brown rice, and enriched cereals to your diet. In part for their carbohydrates, but also they are packed with protein, vitamins, and minerals—meaning they are a complete nutritional package. Whole grains also contain fiber which is known to reduce pregnancy complications like gestational diabetes, constipation, and preeclampsia.
4. Leafy greens
No doubt, veggies are superfoods and a fundamental part of every diet. Eating several servings of green vegetables daily is an easy way to get essential vitamins and minerals like vitamins A, D, E, and K—as well as dietary fiber, calcium, and folate. Incorporate dark leafy greens, such as spinach and kale in your diet to achieve this goal.
5. Folate-rich foods
Folate is an essential B-vitamin. A healthy pregnancy diet must include foods that are rich in folate like bananas, avocados, broccoli, and fortified cereals. Folate prevents neural tube defects—brain, spine, and spinal cord problems—in babies.
You can also opt for folic acid, a man-made folate, available as a supplement. Since nearly half of pregnancies are unplanned, and neural tube defects happen in the first 12 weeks of pregnancy (often before most people realize they are pregnant), the Centers for Disease Prevention and Control (CDC) recommends a vitamin containing 400 mg of folic acid daily for all women of reproductive age.
6. Fatty fish
Your baby needs sufficient amounts of omega-3 fatty acids to support development of the brain and eyes. In addition, pregnant women need omega-3 fatty acids to reduce the risks of preeclampsia and premature labor, increase the baby’s birth weight, and boost mood, which naturally reduces postpartum depression.
Fatty fish like salmon and sardines are loaded with healthy omega-3 fats. If you are concerned about excessive mercury intake, you can opt for fish oil supplement or a prenatal vitamin with DHA instead.
7. Sweet potatoes
Sweet potatoes contain beta carotene, a natural source of vitamin A that your baby needs for optimal development of the eyes, bones, immune system, and for healthy skin. If sweet potatoes aren’t your thing, any yellow or orange fruit or vegetable will do. Think carrots, winter squash, and cantaloupe.
8. Dairy products
Dairy products like yogurt, low-fat milk, and egg yolks not only provide extra protein, they are packed with vitamin D, a nutrient that helps your baby absorb calcium and phosphorus, essential vitamins for building strong bones. You can also add orange juice or fortified cereals to reach your daily quota—or check your prenatal supplements to confirm you’re getting 4000 IU daily.
9. Citrus fruit
Citrus fruits, such as oranges, grapefruit, lemons, and limes, can help you get enough vitamin C during pregnancy. According to the ACOG, pregnant women older than 19 need 85 mg and women younger than 19 need 80 mg daily. Vitamin C helps your body repair tissues, builds immunity, and aids iron absorption. You can also add strawberries, apricots, and guava to your diet—they’re all packed with this nutrient.
10. Seaweed
Seaweed is one of the best natural sources of iodine, a nutrient that expectant moms need 220 mcg of daily. It aids in the production of thyroid hormones, which ensure optimal growth and healthy brain development for your little one. Iodine deficiencies in pregnancy can cause miscarriages, stillbirth, and fetal stunted growth. It can also be a factor in learning disabilities in childhood. If you’re sick of seaweed snacks, excellent iodine sources are also from oysters, shrimp, cod, and iodized table salt.
5 foods to avoid during pregnancy
While some foods are optimal to support your baby’s health, there are some you should avoid for the same reason.
1. Alcohol
Alcohol is off-limits during pregnancy. According to CDC, there’s no available information on an amount that’s considered safe; hence, it’s best to avoid it altogether. The American Addiction Centers suggest that drinking alcohol while expecting is responsible for fetal alcohol spectrum disorders, miscarriages, premature birth, stillbirths, and other physical and mental problems in childhood.
2. High mercury fish
Fish are good sources of omega-3 fatty acids, and the Food and Drug Administration recommends eight to 12 ounces weekly during pregnancy. However, some fish containing high amounts of mercury pass through the placenta and may harm your baby. “Mercury poisoning is detrimental to a growing fetus,” Hunnes says. “The biggest concern is the brain and nervous system of the baby.” Avoid fish that are high in mercury, including swordfish, shark, tilefish, king mackerel, and tuna, as well as raw shellfish and sushi. Replace high-mercury fish with low-mercury seafood like crawfish, crab, tilapia, sardines, and salmon.
3. Unpasteurized dairy
It is not safe to consume unpasteurized milk products like soft cheeses, such as feta, during pregnancy. Soft cheeses may contain harmful microorganisms, such as listeria, which can cause miscarriage, food poisoning, and even fetal death. “Eating unpasteurized foods can be detrimental to your health and the growing baby,” explains Hunnes. “You are prone to foodborne illness, leading to dehydration if you present with diarrhea or vomiting.”
4. Raw and undercooked meat
Like unpasteurized milk, raw and undercooked meat is unsafe during pregnancy because pregnant women are immunocompromised and at higher risk of foodborne illness. Undercooked and raw meat can contain salmonella, listeria, e. coli, and more. Pregnant people are 10 times more likely to get food poisoning from listeria than non-pregnant people. Food poisoning can cause miscarriage, stillbirth, and preterm labor. Other meats to avoid due to high risk of being contaminated with listeria include deli meat and hot dogs.
5. Caffeine
It’s best to limit your caffeine intake to 200 mg daily during pregnancy. That’s equivalent to about two mugs of tea, one cup of regular coffee, or five cans of coke. According to research, caffeine can increase fetal heart rate, breathing rate and awake time. Just remember, caffeine is found in foods like chocolate as well. Dietary sources of caffeine count, too, so count them in your daily calculations.
Other tips for a healthy pregnancy
In addition to eating (or not eating) the right foods during pregnancy, there are additional steps you can take to maximize the health of you and your baby.
Prenatal supplements
When pregnant, your body demands more nutrients than before, and foods may not provide everything you need. “Pregnant women may not meet the high demanding nutritional requirement for a healthier pregnancy and are more likely to fall short of vital nutrients from their regular diet,” says Dr. Boyer. That’s why it’s recommended that all women of childbearing age and expectant mothers take a prenatal supplement to get all of the vitamins and minerals that are vital for healthy fetal development.
Certain foods and medications may interfere with absorption of prenatal supplements. For instance, milk may affect iron absorption, so it’s best to take iron supplements with water. Folic acid and phenytoin (an anticonvulsant) are antagonistic when taken together. Meaning, phenytoin will reduce the amount of folic acid in your blood, and folic acid will reduce blood levels of phenytoin. If you are taking any medications during pregnancy, discuss how they might impact your nutrition and your baby’s health with your provider and pharmacist.
Lifestyle changes
It is crucial to get enough sleep at night, take naps during the day, reduce your stress levels, and remain physically active during pregnancy. Relaxation techniques such as yoga, medication, deep breathing, and prenatal massage can help manage stress. Your exercise doesn’t need to be strenuous, just as much as your body allows—leg stretches, daily walks, and swimming are all great options to help you sleep better and regulate your mood. On top of that, working out can help avoid excess weight gain. Work with your healthcare provider to determine how much weight is safe for you to gain during your pregnancy.
Medication
Sometimes, medications are needed to decrease unpleasant pregnancy symptoms. However, not all medicines are considered safe during pregnancy because they could adversely affect development of the growing fetus. If you have pre-existing chronic conditions like anemia, diabetes, and hypertension do not stop your meds without your doctor’s approval. “Your doctor will recommend taking medication if a particular medicine during pregnancy outweighs its associated potential fetal risk,” says Dr. Boyer. Talk to your healthcare provider and pharmacist before taking any supplement, prescription, or over-the-counter medication during pregnancy.
While avoiding all medications may be optimal, it may be impossible. When needed, opt for pregnancy-safe choices. For symptoms like headaches, Tylenol (acetaminophen) is considered safe for pregnant women. Likewise, for severe cases of nausea and vomiting, ACOG recommends Pyridoxine (vitamin B6) orally, either taken alone or combined with doxylamine, which is also considered a sleep aid. Your healthcare provider will suggest the dose and schedule for these medications depending on the severity of your symptoms.
RELATED: What medications are safe to take during pregnancy?
- Early life nutrition and metabolic programming, Annals of New York Academy of Sciences (2010)
- The importance of nutrition in pregnancy and lactation: lifelong consequences, American Journal of Obstetrics and Gynecology (2022)
- The effects of vegetarian and vegan diet during pregnancy on the health of mothers and offspring, Nutrients (2019)
- The impact of mediterranean dietary patterns during pregnancy on maternal and offspring health, Nutrients (2019)
- Adherence to the Mediterranean diet in pregnancy and its benefits on maternal-fetal health: A systematic review of the literature, Frontiers in Nutrition (2022)
- Lean beef contributes significant amounts of key nutrients to the diets of US adults: National Health and Nutrition Examination Survey 1999-2004, Nutrition Research (2010)
- Nutrition during pregnancy, ACOG (2023)
- The benefits and risks of iron supplementation in pregnancy and childhood, Annual Review of Nutrition (2019)
- Pregnant women have inadequate fiber intake while consuming fiber‐rich diets in low‐income rural setting: Evidences from Analysis of common “ready‐to‐eat” stable foods, Food Science and Nutrition (2019)
- About Folic Acid, Centers for Disease Control and Prevention (2025)
- Omega-3 fatty acids and pregnancy, Reviews in Obstetrics & Gynecology (2010)
- Vitamin A and pregnancy: A narrative review, Nutrients (2019)
- Vitamin D for babies, children, and adolescents, Healthychildren.org (2022)
- Vitamin C and immune function, Nutrients (2017)
- Iodine, The Nutrition Source (2023)
- Risks of substance abuse while pregnant & treatment options, American Addiction Centers (2024)
- Questions & answers from the FDA/EPA advice about eating fish for those who might become or are pregnant or breastfeeding and children ages 1 to 11 years, U.S. Food & Drug Administration (2022)
- The dangers of raw milk: Unpasteurized milk can pose a serious health risk, U.S. Food & Drug Administration (2024)
- Listeria and pregnancy, ACOG (2022)
- Food and medication interactions, HealthyChildren.org (2014)