In a 15-year time frame, the number of Americans taking antidepressants has increased by nearly 65%, rising from fewer than 8% of the U.S. population to nearly 13%. Research suggests people who begin taking antidepressants to help manage their mental health sometimes find they are unable to stop—despite the potentially harsh side effects.
Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed antidepressants, and while they aren’t considered addictive, the side effects of SSRIs can include drowsiness, nausea, insomnia, restlessness, and dysfunctional sexual performance.
For a closer look at the impact antidepressants like SSRIs have on Americans and their most intimate moments, we surveyed 1,000 people who’d recently been treated with either SSRI or non-SSRI antidepressants. Read on as we explore how many users are aware of the sexual side effects of SSRIs and how many believe these side effects are worth it.
Medication for anxiety—and its side effects
Depression ranks as the leading cause of disability around the world in persons aged 15-44, according to the Anxiety and Depression Association of America. Among the most common mental illnesses across the U.S., about 7% of adults have depression. Symptoms may include feelings of sadness, insomnia, fatigue, a weakened immune system, and a higher risk for a heart attack.
Selective serotonin reuptake inhibitors (SSRIs) are the most prescribed antidepressants in America. By increasing serotonin levels in the brain, SSRIs are also sometimes prescribed to help treat other conditions, including anxiety disorders. SSRIs aren’t without side effects, though. Up to 73% of people who take SSRIs experience some type of sexual impact from this class of drugs. While these side effects may decrease after a few weeks on SSRIs, some patients may be intolerant to the treatment.
Awareness of sexual impact with SSRIs
Researchers understand that SSRIs seemingly contribute to sexual dysfunction, but they also admit that measuring the true impact of antidepressants on sex drive and functionality can be difficult. In some cases, sexual dysfunction may predate the introduction of SSRIs as a treatment (sexual dysfunction is also a symptom of depression), or it may be related to some other physical condition. For some patients, every phase of intimacy, ranging from desire to sexual excitement and orgasm, may be inhibited by the use of SSRIs.
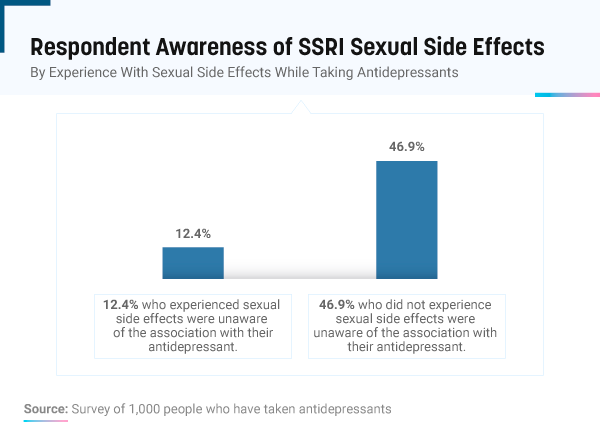
We found more than 82% of people with a history of taking antidepressants were aware of the sexual side effects. Still, many were in the dark regarding how their medication impacted their sex drive and performance. More than 12% of people who experienced sexual side effects on antidepressants were unaware their treatment could trigger the dysfunction, followed by nearly 47% of people with no self-reported decrease in sexual performance.
The importance of physician-patient communication
Communication between doctors, patients, and office staff are a pivotal part of health care. Communication errors, which can be dangerous if not deadly, stem from a lack of understanding, unrecorded conversations, or completely missed discussions. In most cases, miscommunication or missed communication result in errors of medium or high severity.
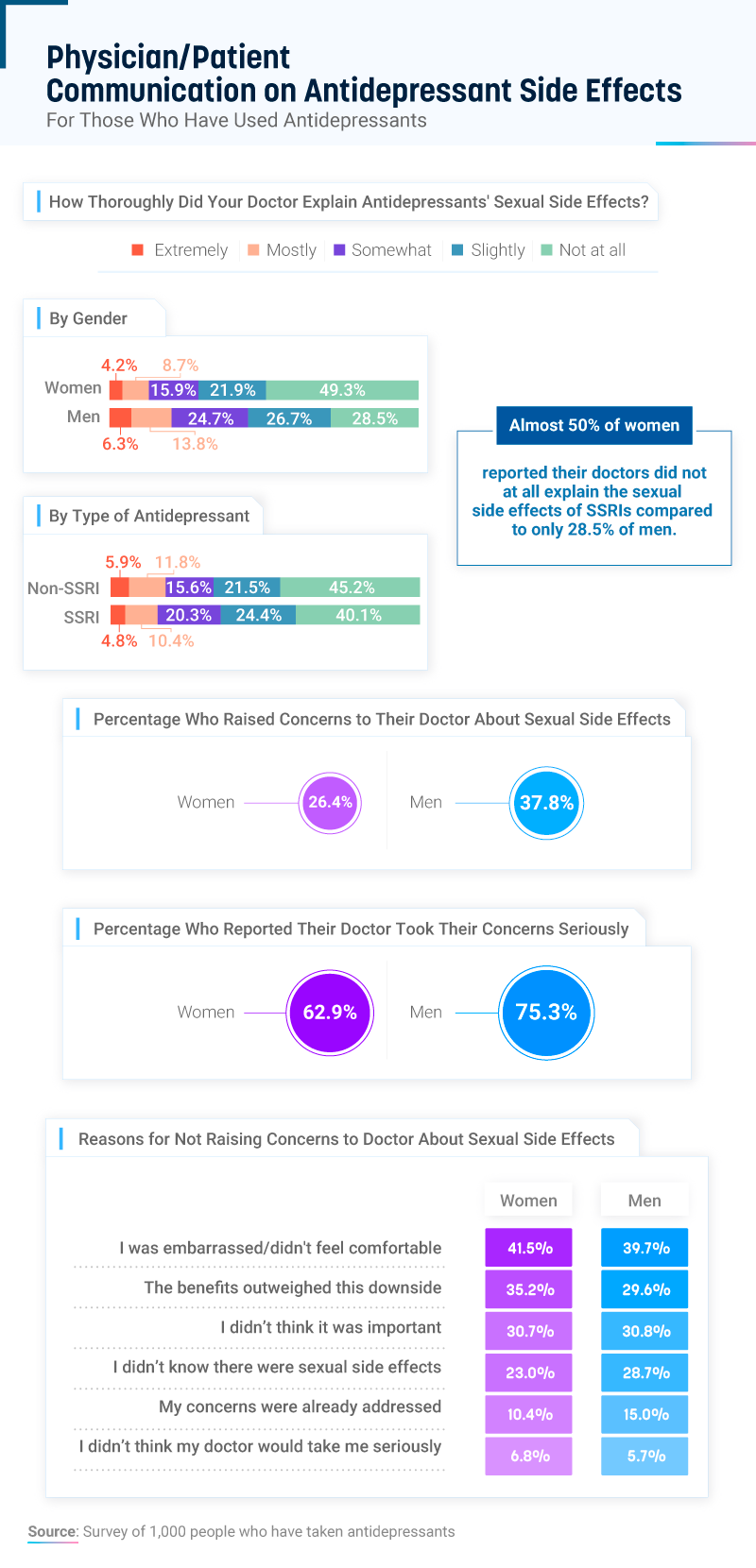
Almost 50% of women and over 28% of men indicated that their doctors did not explain at all the sexual side effects of SSRIs.
While women were more likely than men to receive no explanation from their doctors on the potential for sexual dysfunction, women were also less likely to raise similar concerns to their physicians (26%) or have their concerns taken seriously by their doctors (63%). People with a history of antidepressant use were often too embarrassed or uncomfortable to talk about the sexual side effects of SSRIs with a doctor, followed by people who felt the benefits outweighed the negative impact on their sex life.
Risk and reward: Sexual side effects of SSRIs
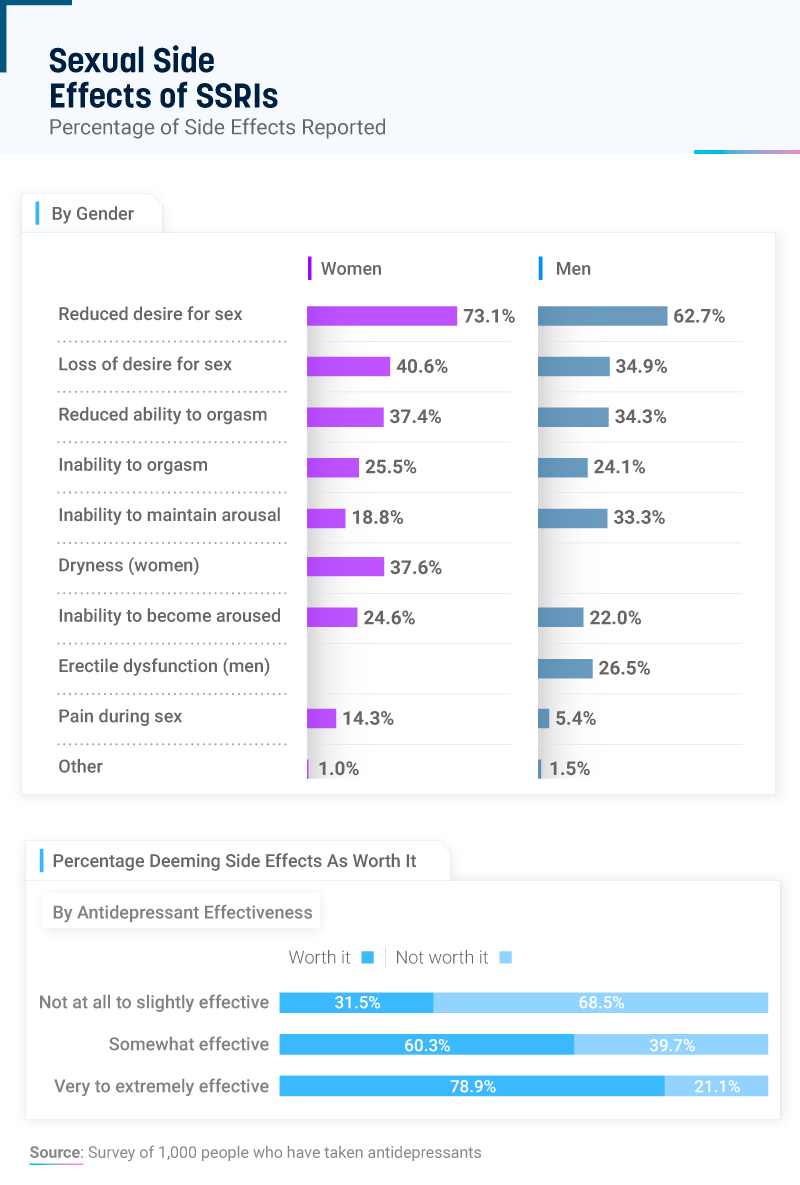
Seventy-three percent of women and almost 63% of men acknowledged feeling a reduced desire for sex while taking SSRIs, and nearly 41% of women and 35% of men said they lost the desire for sex completely. While some fluctuation in sexual desire or intimacy is normal, experts warn that when that desire fades entirely, it can have a negative impact on both relationships and quality of life. Particularly for women, researchers suggest it isn’t uncommon for low libido and depression to overlap.
Women on SSRIs were more likely to report a reduced ability to orgasm, an inability to orgasm, an inability to become aroused, and pain during sex. Still, the more effective that SSRI patients found the treatment, the less concerned they were by the drug’s side effects. Compared to almost 32% of people who believed SSRIs were not at all to slightly effective, 79% of patients who found SSRIs to be extremely to very effective were willing to accept the side effects as being worth it.
The impact of antidepressants on romantic relationships
SSRIs may be the most prescribed antidepressant, but they aren’t the only form of treatment available. Serotonin and norepinephrine reuptake inhibitors (SNRIs), a newer form of antidepressant medication, and norepinephrine and dopamine reuptake inhibitors (NDRIs) also represent potential treatment options. Some antidepressants that don’t affect libido as much as some SSRIs include: Wellbutrin (bupropion) and trazodone.
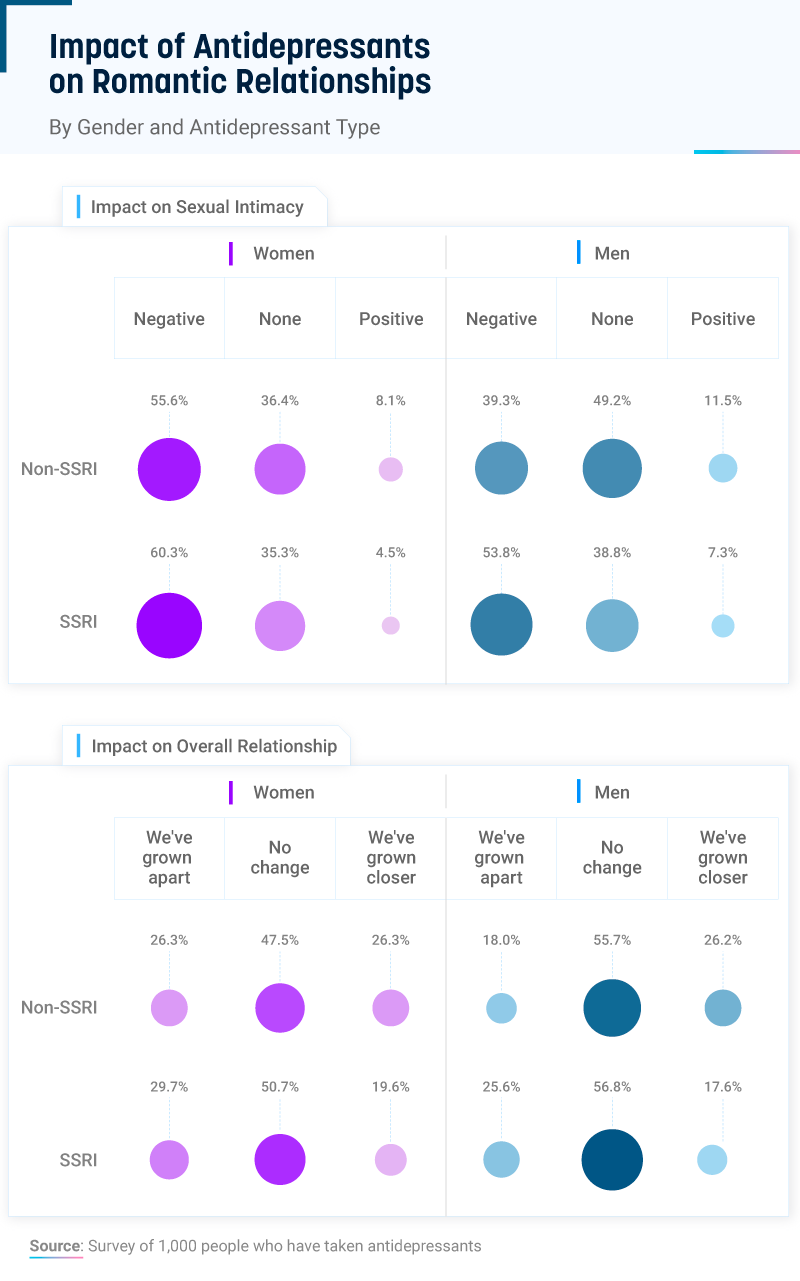
People with a history of antidepressant use were more likely to report worsened sexual intimacy than those on non-SSRIs. Around 60% of women and nearly 54% of men on SSRIs said it hurt their sex lives, followed by 30% of women and 26% of men on SSRIs whose relationships may have grown apart as a result of their antidepressant medication.
Ways to ease SSRI symptoms
Research points to a high correlation between antidepressants and sexual dysfunction, but some solutions allow for a more positive impact of antidepressants. Higher doses often result in a higher risk of sexual side effects, so talking to a doctor about lowering the dosage may help. Taking antidepressants at a certain time of day may also help lower the pressure on sexual activity.
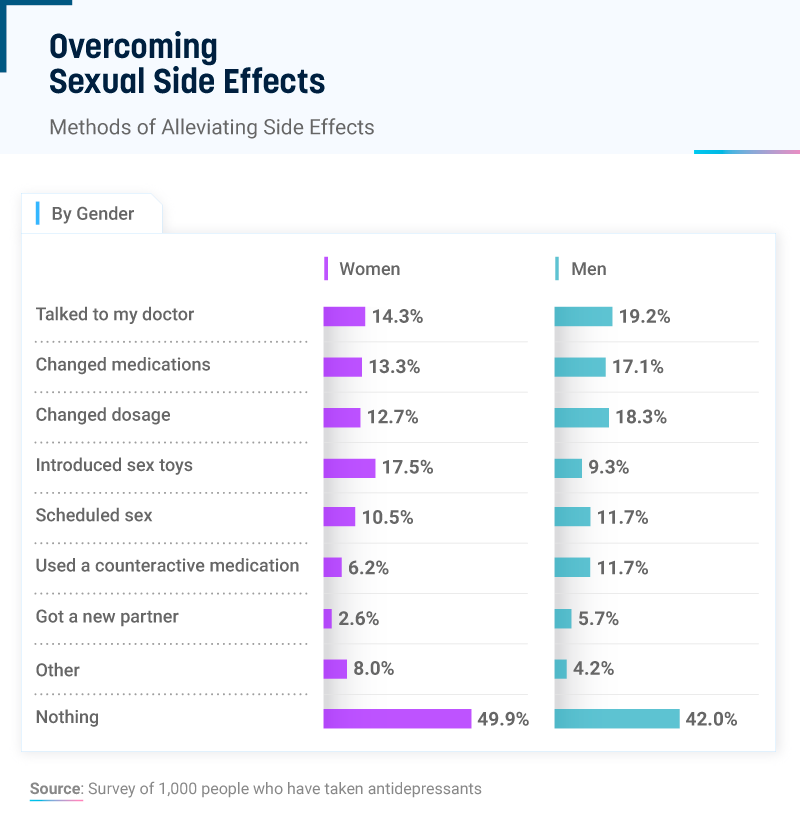
Still, many people chose to do nothing about the effect of SSRIs on their sex life. Fifty percent of women and 42% of men did not attempt to overcome the sexual side effects of their antidepressants, and only 14% of women and 19% of men reported talking to a doctor.
Some people changed medications completely, while others modified their dosage, introduced sex toys into the bedroom, or scheduled sexual activities.
The importance of communication between romantic partners
It can feel as if you have to choose between continuing antidepressants or having a better sex life. However, it’s possible to find a balance between treating depression (or anxiety) without uncomfortable side effects.
Experts recommend increasing communication between romantic partners to avoid unnecessary stress and tension. Adjusting to life on antidepressants can be difficult, and everyone reacts to them differently. Creating an open dialogue between couples can help eliminate additional emotional trauma.
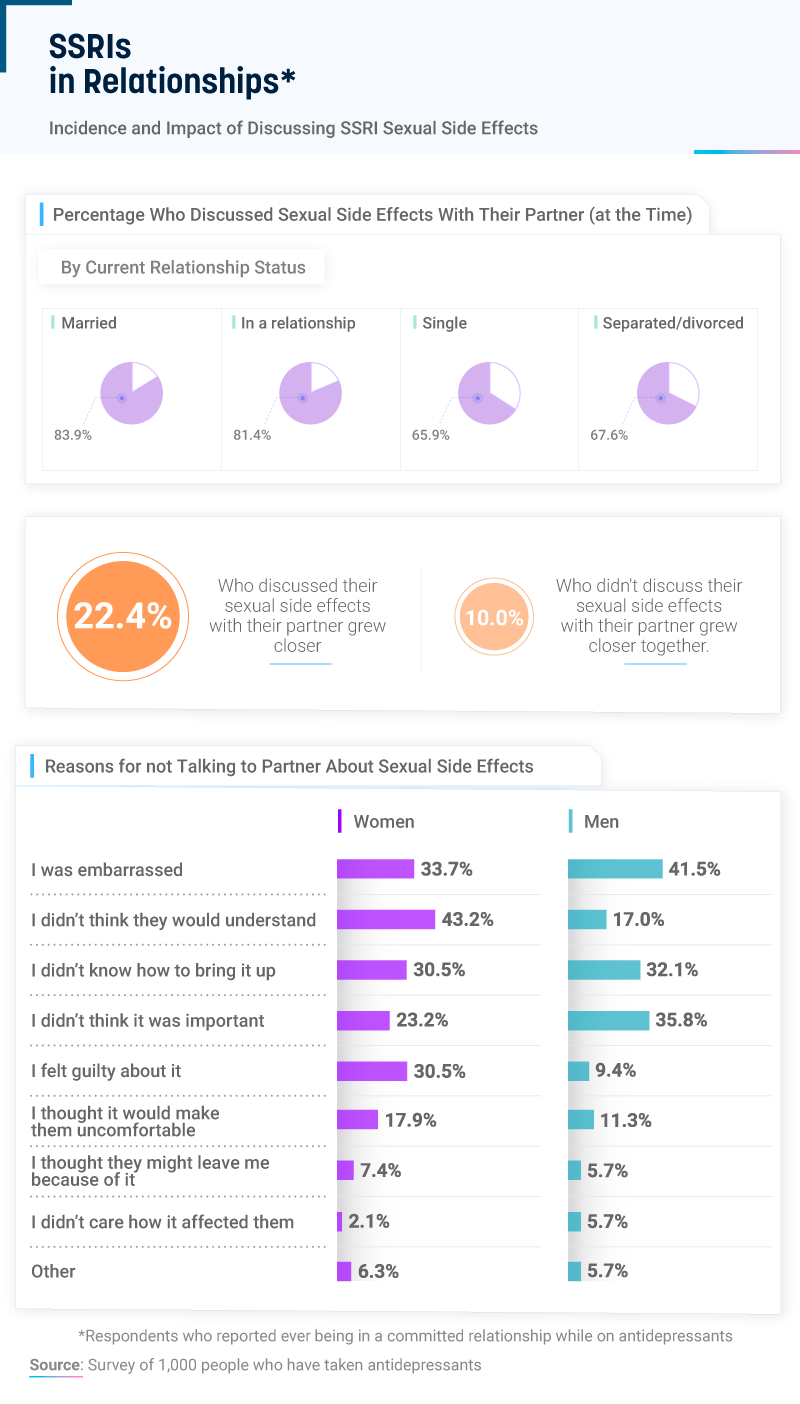
Eighty-four percent of married couples talked about the sexual side effects caused by antidepressants, followed by 81% of people in relationships. While 68% of currently divorced or separated people also opened up to their partners at the time, only 66% of single people shared their experiences on SSRIs. For those who were comfortable opening up about their sexual frustration, more than 22% reported growing closer to their partners, compared to just 10% who didn’t talk to their partner.
Perspectives on mental health
People who had personal experience with life on antidepressants and SSRIs gave us their opinions on how to deal with the sexual side effects.
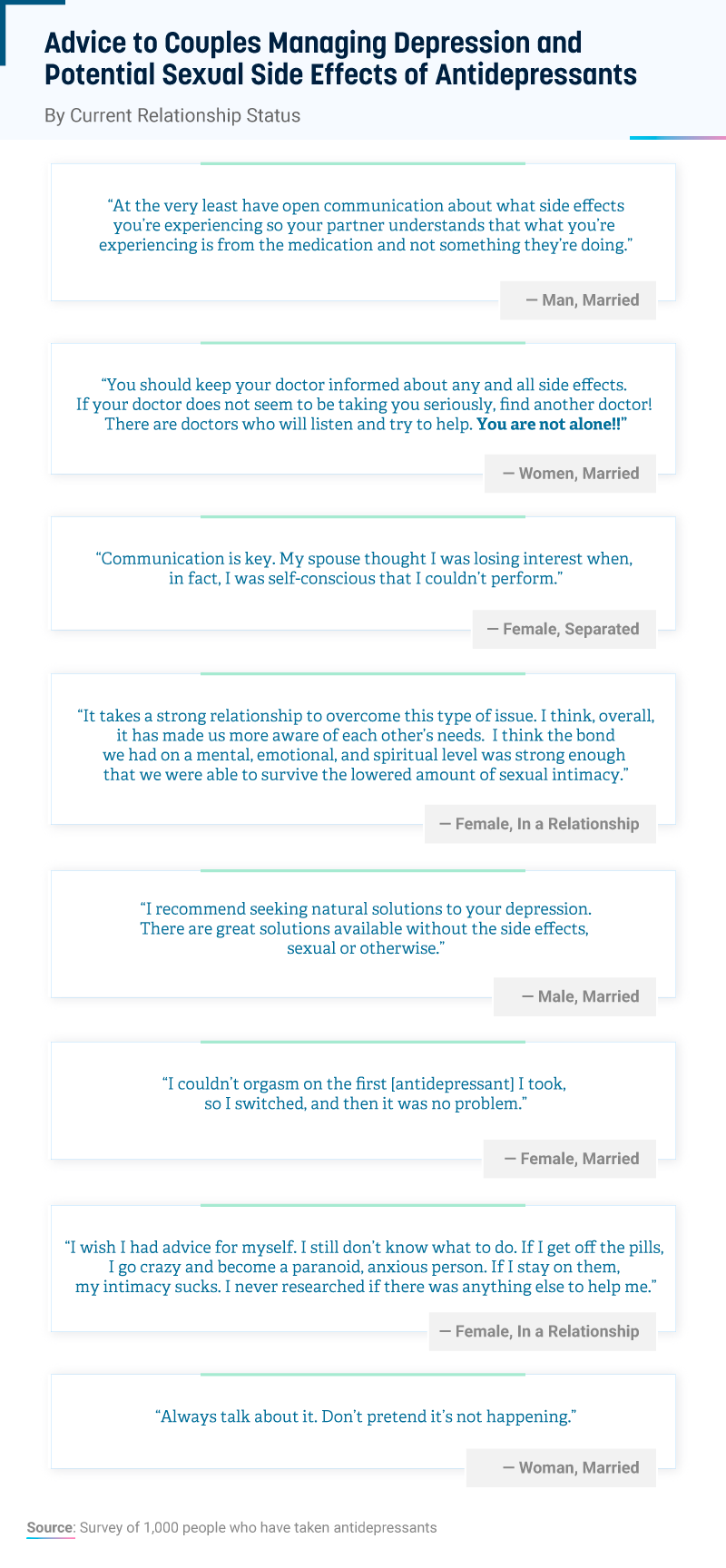
As you can see from their responses, talking about the situation and expressing your feelings was often a recommended course of action. While it can feel daunting or uncomfortable at first, opening up about your sexual experiences as one of you begins treatment can help avoid confusion, assumptions, and hurt feelings.
Additionally, many people acknowledged the importance of sharing these experiences with a physician when experiencing adverse sexual side effects.
Conclusion
More than 16 million Americans have depression, and many of them treat the condition with antidepressants including SSRIs. While these medications may offer much-needed relief, many people report experiencing sexual dysfunction and reduced sexual desire as a result of the treatment. Based on our survey, there appears to be a gap in communication between physicians and patients as to the nature of these sexual side effects, particularly among women.
Whatever medication you use, the cost shouldn’t be an added side effect. At SingleCare, our mission is to make saving on your prescription medications as easy as possible. Use our website or app to find your prescription, compare prices, and save at the pharmacy of your choice.
Methodology
Through Amazon’s Mechanical Turk, we collected responses from 1,002 participants who had most recently been treated with either SSRI antidepressants or non-SSRI antidepressants. 60.3% of our participants were female, and 39.7% were male. Participants ranged in age from 18 to 71 with a mean of 35.7 and a standard deviation of 10.4. Respondents who had not been diagnosed with depression or who had never experienced feelings of depression were excluded from the survey, in addition to those who had not been treated with antidepressants.
The data we are presenting relied on self-reporting. Self-reported data have issues such as selective memory, telescoping, attribution, and exaggeration. Examples of susceptible self-reported data in this study are the one-sided report of antidepressant impact on relational dynamics, as well as experience with side effects. No statistical testing was performed on this data, so the claims listed above are based on means alone.




