Key takeaways
Mirena IUD, used for birth control and treating prolonged menstrual bleeding, releases levonorgestrel, causing common side effects like acne, weight gain, and hair loss, alongside device-related complications.
Common side effects of Mirena include menstrual changes, nausea, abdominal pain, headache, and more, with serious side effects being blood clots, uterine perforation, and ectopic pregnancy.
Device complications can occur, such as migration within the uterus, expulsion, or perforation, with risks being higher shortly after childbirth.
To avoid side effects, provide a complete medical history to the prescriber, check the device’s placement monthly, remove tampons carefully, and report any STIs to a healthcare professional.
Common Mirena side effects | Serious side effects | Acne | Weight gain | Hair loss | Device complications | Side effects timeline | Contraindications | Warnings | Interactions | How to avoid side effects | How to treat side effects
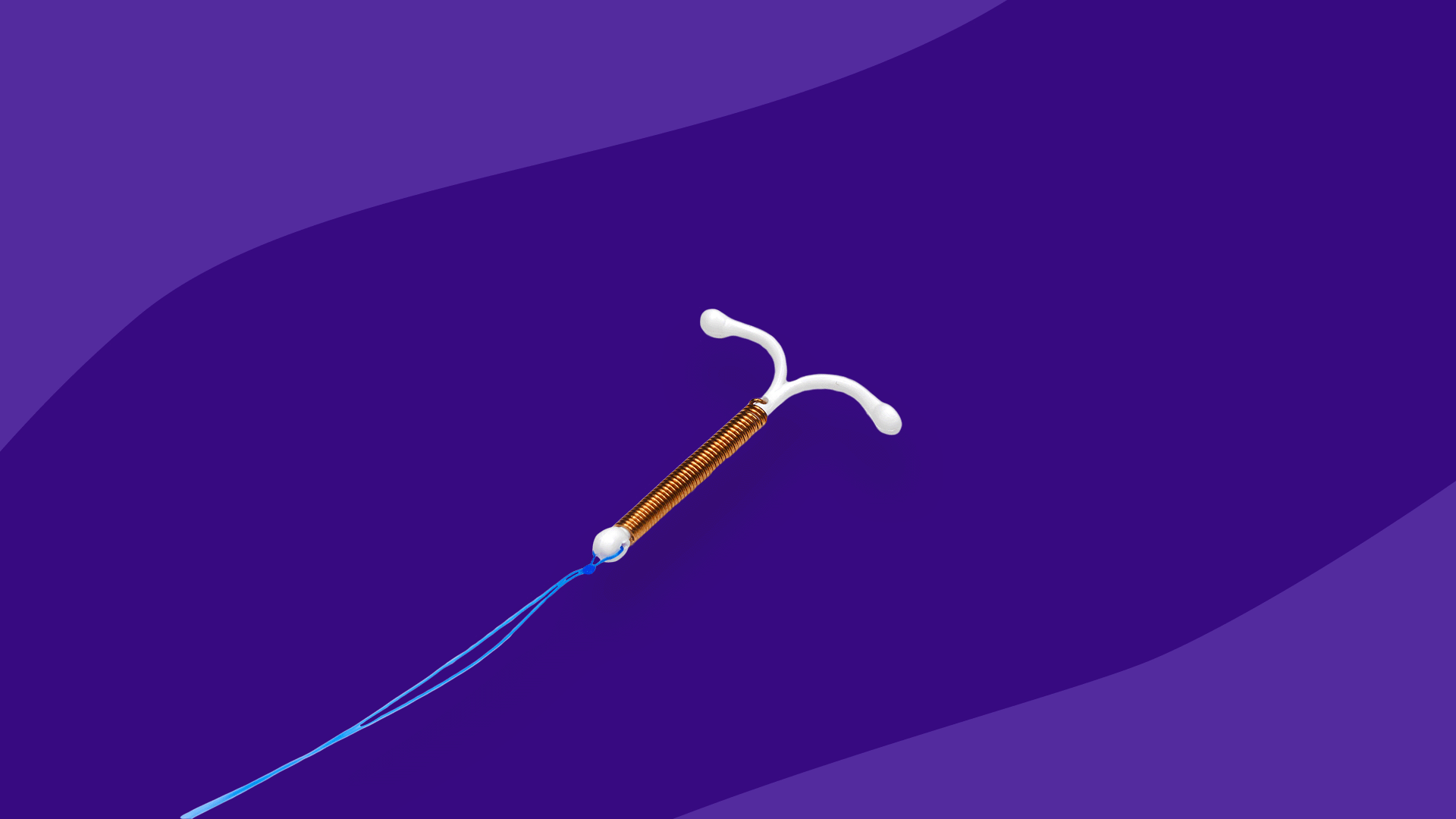
Mirena is a brand-name women’s hormonal intrauterine device (IUD). Mirena provides up to seven years of birth control, but it can also be prescribed to treat prolonged menstrual bleeding for up to five years. Mirena steadily releases levonorgestrel, a progestin hormone, directly onto the uterine lining. By doing this, it both prevents monthly ovulation and changes the lining in the cervix and uterus to prevent sperm movement and egg attachment. Like other hormonal birth control methods, side effects are commonly experienced. Most of these are mild and related to the effects of the hormone.
Common side effects of Mirena
The most common side effects of the Mirena intrauterine system are menstrual changes. Ranging from menstrual cycle irregularities to changes in blood flow, most women will experience one or more of these problems at some point within the months following an IUD insertion. In order of incidence, the most common side effects of Mirena are:
- Altered menstrual periods or irregular bleeding
- Decreased uterine bleeding
- Nausea
- Abdominal pain
- Missed periods
- Headache
- Genital discharge
- Heavy periods
- Genital swelling and infections
- Vomiting
- Breast tenderness
- Back pain
- Pelvic pain
- Benign ovarian cysts
- Acne
- Depression
- Severe menstrual cramps
- Weight gain
- Genital tract bleeding
- Anxiety
- Depression
- Painful intercourse
- Decrease in sexual interest
Serious side effects of Mirena
The most severe side effects of Mirena include:
- Blood clots
- Perforation of the uterus or cervix
- Ectopic pregnancy
- Pelvic inflammatory disease
- High blood pressure
- Sepsis
- Severe allergic reactions
Mirena and acne
In clinical trials, almost 7% of participants reported problems with acne, but the incidence may be as high as 15%. While progestin-only birth control pills are known to cause acne, both hormonal and copper IUDs are most strongly associated with acne. This applies to all women, whether they have acne or not at the time of the IUD insertion. If acne occurs or worsens after an IUD has been inserted, talk to the prescribing healthcare provider for treatment options.
Mirena and weight gain
Weight gain can occur in women who use Mirena over several years. In one clinical study, approximately 9% of women reported gaining weight after six or more years with the device. Six years is a long time, so it’s not clear if the device was responsible for that weight gain. If body weight inches upwards in the years after an IUD has been inserted, talk to a healthcare professional for medical advice.
Mirena and hair loss
Alopecia, or hair loss, is a reported side effect of Mirena, but the incidence is unknown. One study found that 0.33% of women with a levonorgestrel IUD had problems with hair loss. However, 1% of women experienced hair loss in the clinical trials for Kyleena, a levonorgestrel-releasing IUD similar to Mirena and made by the same manufacturer, Bayer. Suffice to say that some women will experience hair loss or hair thinning while using a Mirena IUD. Ask the prescriber for medical advice if hair loss becomes a problem. In most cases, hair loss is reversible if the IUD is removed.
Mirena device complications
It is possible for the Mirena device to migrate within the uterus and either be expelled from the body or end up near the cervical canal. This is a fairly common side effect and usually happens in the weeks or months following its insertion. In more serious cases, the device can either embed itself in the muscles lining the uterus (myometrial embedment) or even cut a hole in the uterus. Perforation is more likely in women who have the device inserted shortly after delivering a baby (0.6%) than in other women (0.1%). In the worst cases, the device can rupture the uterus, migrate into the abdominal cavity, and possibly result in a serious infection. Surgery will be required to remove the device.
How soon do Mirena side effects start?
Side effects, such as cramping, abdominal pain, and menstrual changes, typically start within a few weeks or months after the Mirena IUD has been inserted. Other side effects, such as acne, decreased libido, weight gain, depression, and hair loss, are delayed side effects. They may not be a noticeable problem until several months or years following the insertion.
How long do Mirena side effects last?
Mirena’s most common side effects improve in the first few months. Cramping typically gets better in a few weeks, while menstrual irregularities and ovarian cysts typically last three to six months. Other side effects, such as acne, may require treatment to improve. Most others are reversible when the device is removed.
What are the long-term side effects of Mirena?
The Mirena device can remain in the uterus for up to seven years. The most likely long-term side effects are physical problems with the device. The device can either move to another part of the reproductive tract, be expelled entirely, or break, making it less effective at preventing pregnancy. The device can also puncture or rupture the uterus and even pass from the uterine cavity into the abdomen and other organs. Perforation is most often caused during the insertion, so it’s primarily an early side effect. However, if the IUD is inserted correctly, perforation is typically a delayed or long-term side effect.
Mirena contraindications
Mirena is never used in women with certain medical conditions, including:
- Pregnancy
- Pelvic inflammatory disease (PID), a history of PID, or conditions that increase the risk of PID
- Any history of uterine lining swelling immediately following a pregnancy
- Uterine or cervical cancer
- Breast cancer or other hormone-sensitive cancers
- Abnormal vaginal bleeding
- Untreated swelling or infection of the cervix or vagina
- Uterus irregularities such as fibroids
- Liver disease or liver tumor
- An unremoved IUD
- Incomplete abortion
- Infected abortion
- Allergies to any part of the IUD or its medicine
Mirena is never used as emergency contraception.
Pregnancy
Mirena is contraindicated during pregnancy and is never inserted if a pregnancy is known or suspected. If a woman becomes pregnant, the Mirena device will probably be removed, but the procedure risks ending the pregnancy. Leaving Mirena in place during pregnancy increases the risk for infection, sepsis, miscarriage, and premature birth. In rare cases, babies have been born with birth defects when an IUD remains in the uterus. If the fetus is female, it can be born with male sexual characteristics because of its elevated exposure to the progestin hormones released by the device.
Breastfeeding
Mirena can be inserted in women who are breastfeeding. However, healthcare providers are urged to wait at least six weeks after the baby has been delivered before inserting the device because of the higher risk of perforation. Levonorgestrel crosses into breast milk, but no problems have been reported in nursing infants.
Children
Mirena is FDA-approved to be used in any woman of any age following the first period.
Seniors
Mirena is only used in women of reproductive age.
Mirena warnings
Mirena may not be right for everyone. Aside from contraindications, some medical conditions increase the risk of problems. As a result, healthcare providers may be cautious about inserting a Mirena device or may have to watch more closely for side effects or other issues.
Cautions
Because of possible device risks, such as perforation of the uterus, Mirena use is generally avoided, but not prohibited:
- Within six weeks of delivery of a baby
- Before the uterus has returned to normal following pregnancy
- When a uterus is oriented backward rather than forward (retroverted uterus)
Because of possible complications during the insertion procedure, healthcare providers may take extra measures performing an insertion in people with:
- Seizure disorders
- Slow heartbeat
- A history of fainting
- Bleeding problems
Because of possible adverse effects, healthcare providers may need to monitor women who have:
- A history of ectopic pregnancy
- Blood clots or a history of blood clots
- Risk factors for blood clots such as:
- Severe arterial diseases such as stroke or heart attack
- High blood pressure
- High cholesterol
- Lupus
- Smoking
- Diabetes
- Migraines or severe headaches
- Weakened immune system
Abuse
The Mirena IUD is not subject to abuse, nor does it cause physical dependence.
Overdose
The Mirena device delivers a steady, small dose of levonorgestrel throughout the day. An overdose is not likely. The only way to tell, however, is through side effects. Contact a healthcare provider or call a poison control center if a cluster of unusual side effects suddenly manifests, including headache, nausea, vomiting, abdominal pain, breast tenderness, or unusual vaginal bleeding.
Mirena interactions
Drug interactions are not a serious problem with Mirena. Although the levonorgestrel released from the device enters the bloodstream, its contraceptive effects are due to the drug’s direct contact with the uterus. Drugs that affect the breakdown of levonorgestrel in the body will reduce the effectiveness of other forms of hormonal birth control, such as birth control pills, but are unlikely to compromise the effectiveness of a levonorgestrel IUD.
Still, some drugs should not be used with an IUD. These include:
- Mifepristone: The combination of mifepristone and misoprostol to terminate a pregnancy is contraindicated in people with an IUD.
- Blood thinners increase the risk of bleeding during the insertion procedure.
How to avoid Mirena side effects
Hormonal contraception commonly produces side effects—usually changes with the menstrual cycle, irregular bleeding, mood changes, and cramps. However, the IUD itself may cause problems if it moves or punctures the uterine wall. A few tips can help.
1. Give the prescriber a complete medical history
For hormonal IUDs, the most effective way to prevent side effects is to make sure the prescriber has a complete medical history. Make sure to tell the prescriber if you:
- Already have an IUD inserted
- Are or think you may be pregnant
- Have recently had a baby
- Have or ever had a serious pelvic infection
- Have an untreated genital infection
- Have cancer
- Have vaginal bleeding that can’t be explained
- Have had a heart attack or stroke
- Have heart valve problems
- Have any problems with blood clotting
- Have high blood pressure
- Get migraines or really bad headaches
- Have liver disease
- Have HIV/AIDS or other sexually transmitted infections (STIs)
- Smoke, use drugs, have multiple sexual partners, or have immune system problems
2. Check the device’s placement
Check the placement of the device once per month. A healthcare provider will teach you how to do this. Each device has threads that are meant to protrude from the cervix into the vagina. Those threads can be felt by inserting a finger into the vagina. If they’re not there or the threads are too long, the device may no longer be in place. In those cases, see a healthcare provider.
3. Remove tampons carefully
Be careful when removing tampons in order to not to pull on the removal threads of the IUD.
4. Tell the prescriber if you get a sexually-transmitted infection (STI)
Mirena and other intrauterine contraception devices do not prevent sexually transmitted infections. If you or your partner acquire an STI (including HIV/AIDS), inform a healthcare professional. An STI increases the risk for pelvic inflammatory disease, so the Mirena device may need to be removed.
How to treat side effects of Mirena
Many of Mirena’s side effects can be handled at home or will go away on their own. Some, however, may require medical attention.
Cramps
Ask a healthcare provider for medical advice on treating cramps at home. Ibuprofen should be okay to use, as long as there are no present contraindications to it. Cramps are usually at their worst in the weeks following insertion, but they improve over time. If cramps continue for a long time or become severe, talk to a healthcare professional.
Pelvic infection
Get medical attention at any sign of a pelvic infection, including pain in the lower abdomen, heavy vaginal bleeding, unusual vaginal discharge, pain during sexual intercourse, fever, chills, or sores on the genitals.
Pregnancy
Immediately talk to the prescribing healthcare provider if you become pregnant or think you may be pregnant.
Perforation
If the device pierces the uterine lining, medical attention is needed. The usual signs of perforation include sharp abdominal pain and vaginal bleeding. Both of these are common side effects in the first few months after an IUD is inserted. If they happen after the device has been in the uterus for a few years, talk to a healthcare professional. However, about one in three women will not have symptoms. One possible way to tell in those cases is if the removal threads are no longer in place. The prescribing healthcare provider should always be informed if the threads have moved.
Expulsion
Sometimes part or all of the device comes out of the uterus. If it’s not noticed when it comes out, it can be indicated by symptoms such as pain or bleeding. Immediately call the prescriber. Abstain from sexual intercourse or use a backup method of birth control, such as a barrier method with spermicide.
Sources
- Hair loss with use of the levonorgestrel intrauterine device, Contraception
- Influence of contraception class on incidence and severity of acne vulgaris, Obstetrics and Gynecology
- Intrauterine device migration, MDEdge Emergency Medicine
- Kyleena prescribing information, U.S. National Library of Medicine
- Mifepristone prescribing information, U.S. National Library of Medicine
- Migration of intrauterine devices: Radiologic findings and implications for patient care, RadioGraphics
- Mirena, Epocrates
- Mirena drug summary, Prescriber’s Digital Reference
- Mirena HCP website, Bayer
- Mirena prescribing information, U.S. National Library of Medicine
- Mirena website, Bayer