Key takeaways
Following the 5 Rights of Medication Administration (right drug, dose, time, route, and person) is crucial for the safety and health of cancer patients.
Effective cancer medication management involves maintaining a detailed medication list and ensuring safe storage and handling, particularly with hazardous medications like chemotherapy drugs.
Home treatment of cancer, including at-home injections or intravenous treatments, requires proper training and equipment, and consistency with pharmacies and doctors is advised for optimal care.
Side effects of cancer treatments, such as cognitive impairments and physical discomforts, should be closely monitored and discussed with the care team to adjust medication plans as necessary.
For cancer patients, medication can be a critical aspect of treatment and recovery. Patients often work with a healthcare team who can prescribe the most appropriate medications based on factors like the severity of the cancer, symptoms, and patient preferences.
Since a patient may be on many medications at once and deal with frequent changes to the treatment plan, it’s important to carefully track medicine storage and dosage. Medications work best when taken in the proper doses at the correct times. This guide offers helpful tips for how to manage medication tasks, along with key things to keep in mind when it comes to cancer medication.
What are the 5 R’s for medication safety?
Caregivers who follow the 5 Rights of Medication Administration will be the most effective at keeping cancer patients safe and healthy. These are the same steps followed by the care professionals at a clinic or hospital.
- Right drug
- Right dose
- Right time
- Right route
- Right person
Right drug
If you’re a patient administering a drug, first make sure you’re using the correct one. Look at the pill bottle, then read the name of the drug out loud.
Right dose
A common cause of dangerous adverse drug events is giving an improper dose. This mistake usually happens when caregivers misread or mismeasure the proper amount.
Right time
A medication plan will only be successful if the proper medication is given at the right time. One of the best solutions is a written medication schedule.
DOWNLOAD THIS TEMPLATE FOR FREE
Right route
Cancer medications can be administered as pills, liquids, topical treatments rubbed on the skin, and injectable treatments. Injectable treatments include intravenous (IV) infusions or injections through the vein, intramuscular (IM) injections into the muscle, and subcutaneous (SQ) injections under the skin. Follow the directions given with the medication, and ask for help if you feel you need it.
Right person
Pill bottles can look very similar. As a last step before administering the medication, look again at the medication to make sure it’s being administered to the right person.
General tips for effective cancer medication management
Two important strategies will help you give medication safely throughout the treatment process: keeping a medication list and storing medication properly. Medication storage and handling is especially important because some treatments may be hazardous.
Medication list
A medication list is a critical document that will be consulted by patients, caregivers, pharmacists, and doctors. Make sure to add any supplements or over-the-counter medications to the list in addition to prescribed medications.
The medication list should include the name of the medication, the dosage or how the medication is taken when treatment with the medication began, and any concerns such as side effects experienced.
Safe storage and organization
Cancer medications are powerful and very dangerous if taken by the wrong person or handled improperly.
If anyone at home is at risk of accidentally ingesting them (like a child, other family members, or a pet), make sure to store the pills in a high place they cannot reach. You may also want to invest in a pill lockbox. Do not store cancer medications in the bathroom—the humidity can lessen their effectiveness.
Ideally, only the person who is taking the medication will touch it. If a caregiver needs to handle the medication, they should only do so while wearing gloves.
Hazardous at-home medications
If any of the medication being taken at home is hazardous, such as chemotherapy drugs like doxorubicin or vincristine, caregivers will need to take additional safety steps.
Caregivers should be given special kits with instructions and materials for cleaning spills and special containers for disposing of hazardous medications.
These medications can still be present in dangerous amounts in bodily fluids, such as urine, blood, saliva, etc. If any of these fluids are present on the patient’s bed sheets, towels, or clothes, handle them with disposable medical gloves, and wash the soiled fabrics in hot water separately from other laundry.
Special care should be taken when using the toilet. For 48 hours after an injection or IV treatment, the patient should flush the toilet twice after use, wash their hands well, and cleanse any body parts that have urine or feces on them. Be careful when handling and throwing away disposable undergarments. The toilet water could still contain trace amounts of hazardous chemicals, so children and pets should be kept away from the bathroom.
Powerful cancer drugs, like any medication, must be taken at the proper time in order to be the most effective. Missing scheduled dosing times completely or taking pills at the wrong time could be dangerous.
To make sure you administer all pills at the proper time, set reminder alarms on an alarm clock or timer. If you have a smartphone, consider using an app designed for medication management.
It’s also a good idea to write down the daily medication plan on a sheet of paper. A physical list can be easily copied and shared with other caregivers and health aides, and you don’t have to worry about phone compatibility or a data outage making the medication plan inaccessible. It can easily be tucked into the inside pocket of a purse or wallet.
Having a record of daily medications is also very helpful at follow-up appointments with the patient’s care team. These appointments are the ideal time to discuss adjustments in medication timing that may help reduce side effects experienced. You may discuss moving the timing of a treatment dose closer to a mealtime, for instance, or further away from bedtime. These are just examples. Never make any changes to a medication plan without first discussing them with the assigned care team.
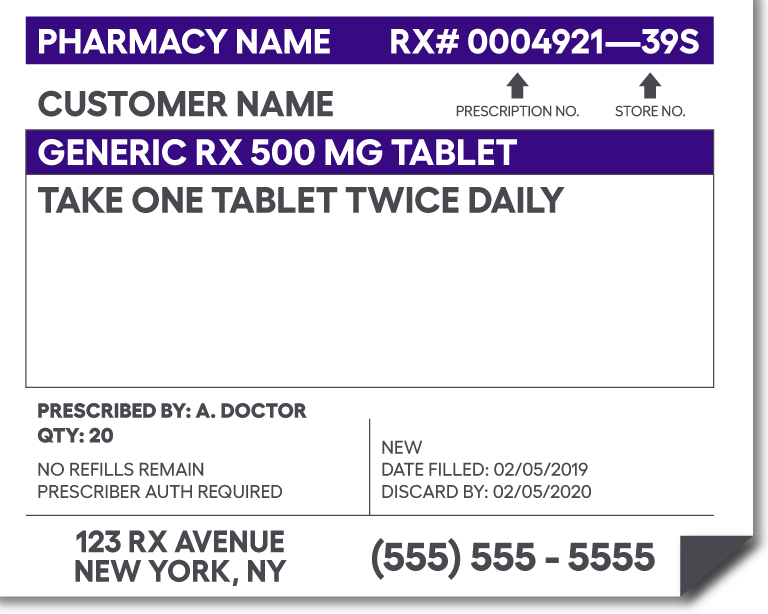
Understanding the prescription bottle label
Typically, a prescription label has eight parts and types of information. Keep in mind that your own prescription labels may look somewhat different, but they will generally have similar content listed for you to reference. Learn to recognize these parts on medications.
- Pharmacy information: Key details about the pharmacy that filled the prescription
- The patient’s information: Contact information of the patient
- Prescribing doctor’s information: Contact information of the physician or healthcare provider
- Drug name and strength: Brand, chemical, or generic name along with the measured amount of one unit of the medicine
- Instructions on taking the medicine: How and when to take the medication
- Prescription information: Specific information to aid in planning for refills
- Pharmaceutical manufacturer information: Name of the company that manufactured the medication and a physical description of the drug
- Federal caution statement: Prescription warnings mandated by the U.S. government
Many prescription medications also come with medication guides that are approved by the Federal Drug Administration (FDA). These guides have information about issues specific to particular drugs and may help patients avoid serious side effects.
At-home injections or intravenous treatment
When it is safe to do so, chemotherapy treatment can be given at home. A home health aide will do the procedure or train a caregiver to do so.
If a home care nurse is administering these treatments at home, they will be responsible for learning about and caring for the many types of special equipment, like the tubes, lines, ports, and catheters that are used in cancer treatment. Someone at the cancer care facility will train the home health aide or caregiver about the specific equipment before the patient starts any at-home treatments.
Avoid switching pharmacies or doctors
Cancer treatment is a complex process. The care team often weighs many factors in developing a medication plan, including the patient’s past medical history, allergies, type of cancer diagnosis, the stage of the cancer, and others.
Because the process is so involved, it’s best to stay consistent with the pharmacy you’re using and the doctors you’re seeing. That means sticking to one pharmacy for all medications, if possible. This increases the likelihood that a pharmacist will catch errors and be able to advise on ongoing medication regimens when asked.
Active treatment and maintenance therapy
Many cancers are treated with the goal of eliminating it from the body. When treatment is in this stage, it is sometimes called active treatment or maintenance therapy. In a best-case scenario, the patient is completely free from cancer at the end of treatment.
Some cancers are chronic in nature. They cannot be fully cured; they’re only managed with ongoing chemotherapy to keep the cancer from spreading or worsening. Such cancers may include ovarian cancer, some leukemias, and some lymphomas.
Once treatment has successfully reduced the signs and symptoms of the cancer, the disease is said to be in remission. When the cancer isn’t growing, it may be called “controlled” or “stable.” Growing cancers are often described as in the progression phase. If a chronic cancer begins progressing, treatment may need to be resumed.
Homeopathic, alternative, or complementary cancer treatment
Hospitals and cancer care facilities take an evidence-based approach to treatment. The cancer treatments recommended by doctors have proven effective in clinical trials of cancer patients.
There are other treatments that are not proven to eliminate cancer but can relieve some symptoms of the disease. Meditation may help reduce anxiety. Tea may assist digestion or reduce nausea. Massage or acupuncture may help relieve pain. Cancer treatment professionals may encourage the use of these therapies when used in conjunction with evidence-based treatments, such as pain medication or radiation therapy.
Side effects
The side effects of cancer treatment can affect a patient’s ability to stick to their medication plan. For example, the American Cancer Society mentions confusion or delirium as a serious side effect associated with cancer treatments and pain-relieving drugs. Less serious cognitive lapses during cancer treatment—like forgetting names or dates or a general feeling of mental cloudiness—are sometimes called “chemo brain.” A patient who isn’t thinking clearly may have a harder-than-usual time remembering to take medication.
Chemotherapy can affect the entire body. Common side effects of cancer treatment include general fatigue, hair loss, constipation, diarrhea, and mouth sores, among others. Other side effects, such as nausea, taste and smell changes, and difficulty swallowing, can make taking medication unpleasant.
Discuss side effects with the care team or home healthcare professional. If side effects are so severe that the medication can no longer safely be taken, healthcare providers may adjust the dose or type of medication.
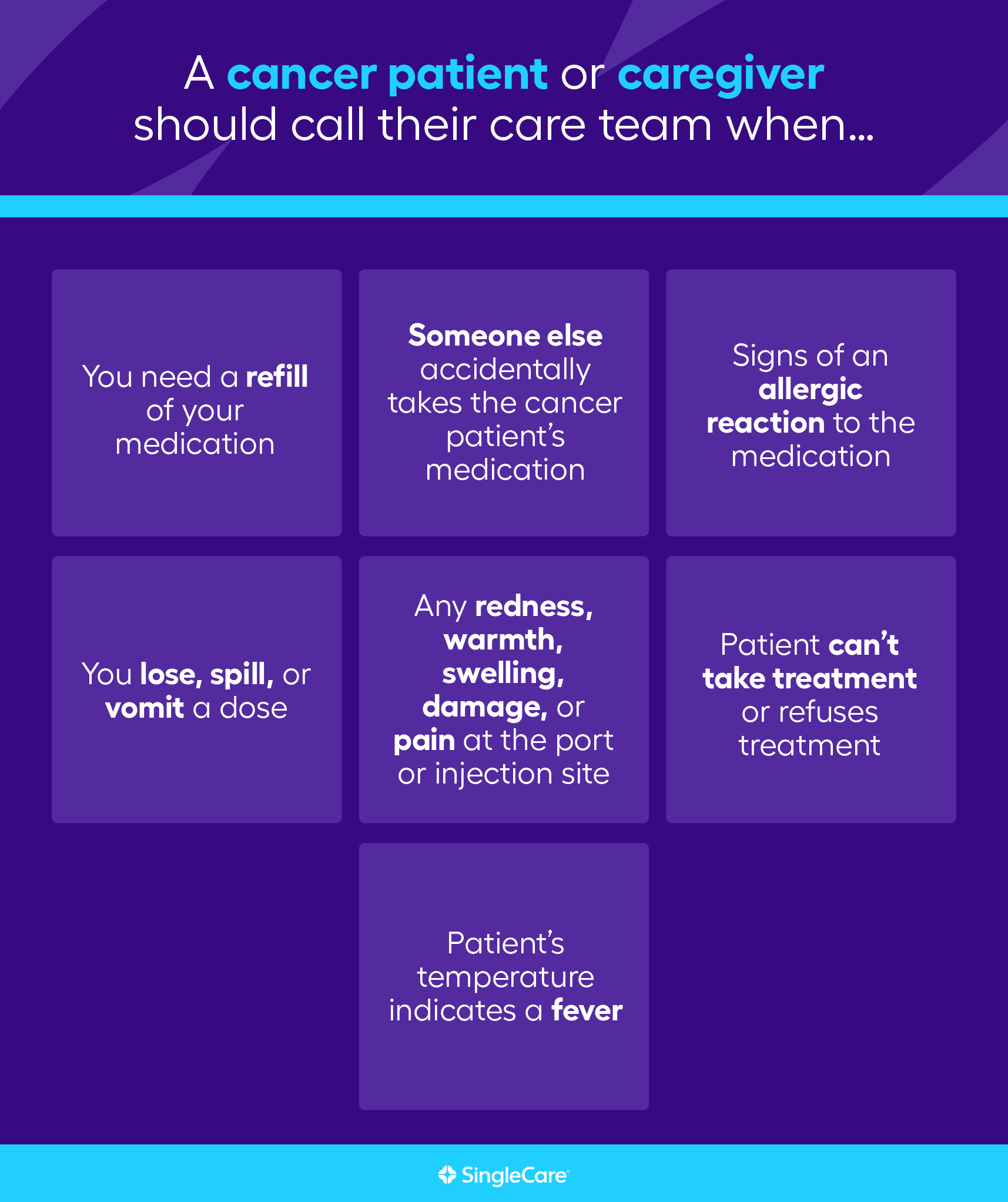
When to immediately contact your medical team
During most cancer treatments, the patient spends the majority of their time at home. Many medical issues that happen at home can be handled by the caretaker or the patient themselves. But if any of these events occur, reach out to the care team.
- You need a refill of your medication
- You lose, spill, or vomit a dose
- Someone else accidentally takes the cancer patient’s medication
- Any redness, warmth, swelling, damage, or pain at the port or injection site
- Fever
- The patient can’t take treatment or refuses treatment
- Signs of an allergic reaction to the medication
Safe disposal of cancer-related treatments
With any medication, safe disposal is important. Medications are powerful chemicals that are dangerous if accidentally ingested or if they get into the soil or groundwater.
Cancer medications are often extremely hazardous. Your care team should give you specific instructions for disposing of these medicines and dispensing equipment safely if they’re no longer needed. You may also get special equipment like a biohazard container. You should not try to figure out how to dispose of a cancer medication. If you weren’t given specific instructions or don’t remember what the instructions were, call your care team and ask for help.
Cancer is scary, but medication management doesn’t have to be
Aggressive cancer treatment can be a life-altering experience. Pills, needles, and intravenous tubes may temporarily become as regular a part of your life as the daily mail. For family caregivers, you’ll be assuming a new role as a part-time nurse. But you have a team of dedicated, full-time medical professionals behind you. The healthcare team will help figure out the best home treatment plan for the patient based on their diagnosis, availability, and skills. Educate yourself by reading guides like this one, but don’t hesitate to ask for help. You can do this.
Sources:
- The five rights, Pharmacy and Therapeutics (2010)
- A to Z list of cancer drugs, National Cancer Institute (2023)
- Managing medications during cancer treatment, MD Anderson (2023)
- Medication storage temperature guidelines, Bay State Health, (2023)
- Cancer drug therapy—safety at home, Roswell Park (2021)
- Medication guides, FDA (2023)
- IV treatment at home, MedlinePlus (2022)
- What is maintenance therapy, American Society of Clinical Oncology (2022)
- Complementary and alternative medicine, National Cancer Institute (2023)
- Managing cancer-related side effects, American Cancer Society (2023)
- Confusion and delirium, American Cancer Society (2021)