Key takeaways
Approximately 21% of adults report living with chronic pain, according to the National Institutes of Health.
Due to the risks of opioid use, such as dependency and overdose, safer pain management alternatives have become essential.
There were more than 80,000 opioid-related deaths in 2022, according to the CDC.
Non-medication pain management techniques include physical therapy, chiropractic care, acupuncture, and massage therapy.
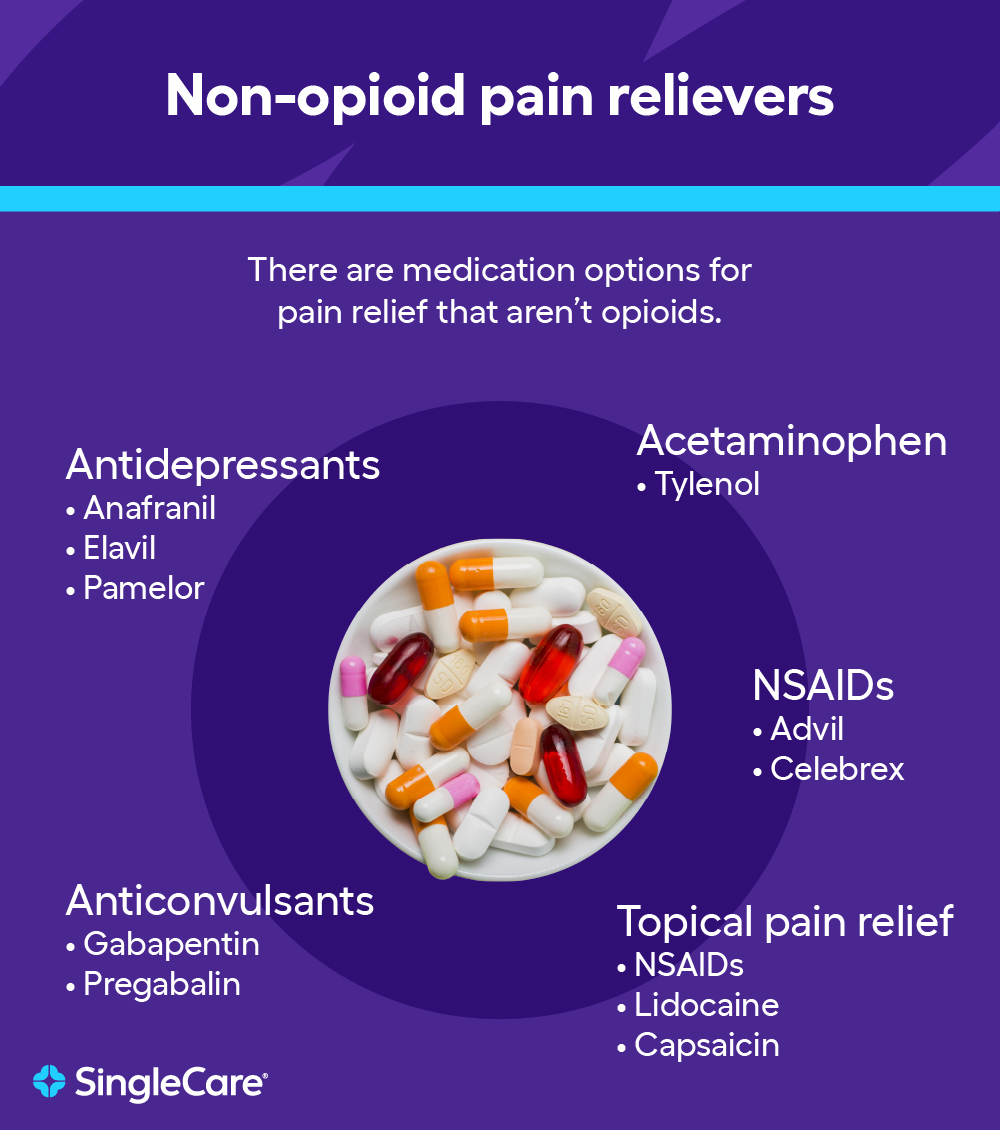
Non-opioid pain medications include NSAIDs (ibuprofen), Tylenol (acetaminophen), antidepressants (such as amitriptyline), anticonvulsants (gabapentin or pregabalin), and topical pain relievers (lidocaine or capsaicin).
Nerve blocks, spinal cord stimulation, and intrathecal drug delivery may be required for persistent pain.
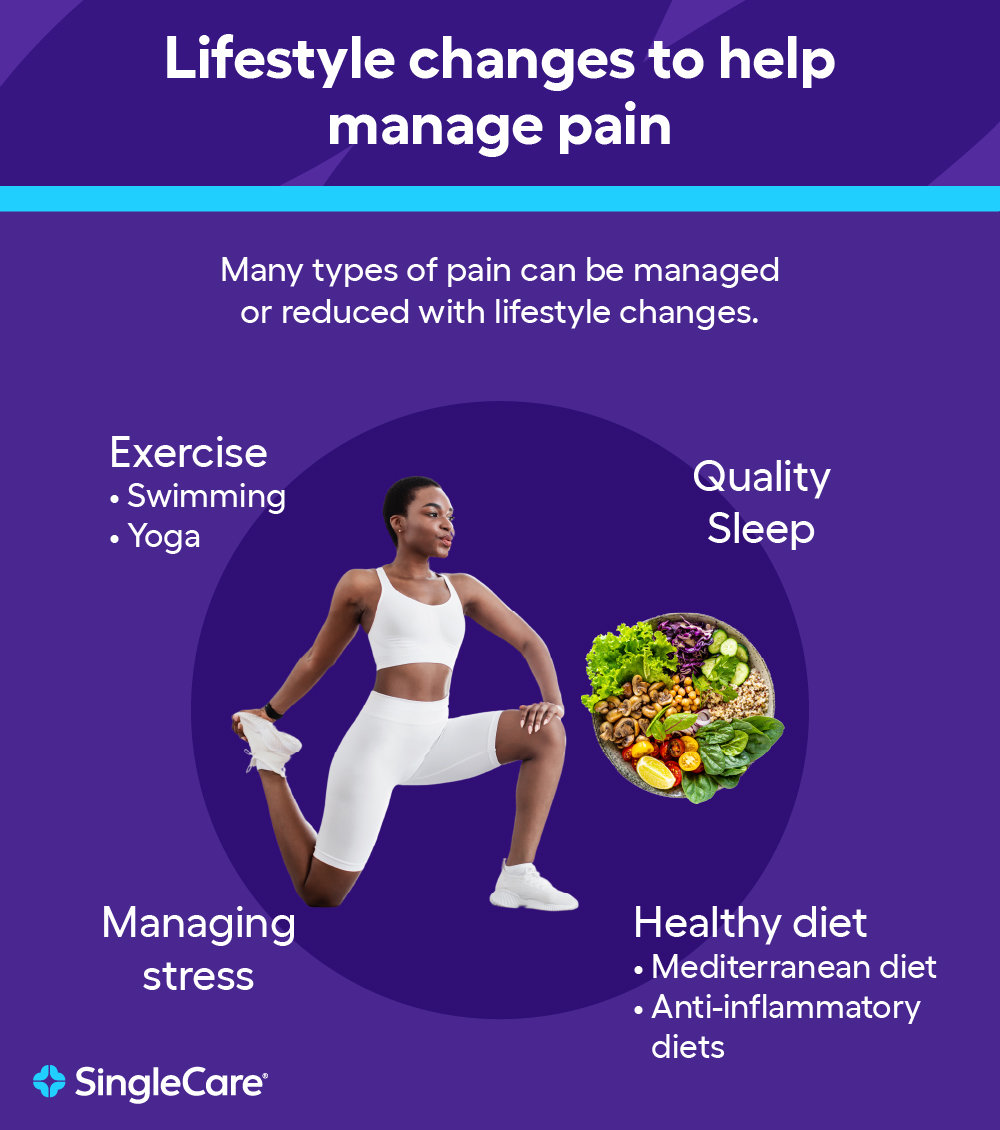
Lifestyle changes such as exercise, a healthy diet, proper sleep, and stress management can significantly alleviate chronic pain and reduce inflammation.
Pain affects all aspects of a person’s life. When it becomes unbearable or significantly affects day-to-day functioning, patients may seek out opioid medications. However, these come with risks, including dependency and overdose. Fortunately, opioid alternatives now offer effective pain management without these dangers.
Why seek alternatives to opioids?
Opioids were once a go-to solution for quick pain relief but come with risks, like dependency, misuse, and overdose.
With the Centers for Disease Control (CDC) reporting over 80,000 opioid-related deaths in 2022, safer alternatives are more crucial than ever.
Acute pain vs. chronic pain
Pain treatment depends on whether it’s acute (lasting less than a month, often caused by injury or surgery) or chronic (lasting three or more months, often requiring long-term care), as described in Pain and Therapy. A 2023 study by the National Institutes of Health found that the rate of chronic pain in adults is about 21%.
Non-medication pain management techniques
Opioid medications only temporarily mask the pain and do not treat its underlying causes. This means pain returns when a patient stops using the medication. This is especially problematic for chronic pain, where patients often become tolerant to opioids, which results in a dose escalation over time, often up to a 10-time increase.
The CDC strongly recommends the use of non-medication pain management techniques for this reason. If medicine is necessary, non-opioids are preferred. Opioids should only be considered if the benefits outweigh the many risks. Fortunately, there are a variety of non-medication options to help manage pain and, in some cases, treat the underlying cause.
Physical therapy
Massage is effective for back, hand, neck, and knee pain. It may also help improve sleep and reduce anxiety and depression symptoms. According to the American Massage Therapy Association, acute pain may resolve after one or two sessions of massage therapy. However, people with chronic pain may require weekly sessions for several months or even years.
Physical therapy does not always require a licensed physical therapist or a healthcare provider—patients can often perform physical therapy by themselves at home using active exercises.
Preventive physical therapy also prevents more severe injuries, especially in patients suffering from only mild pain. A 2018 study showed that patients who saw a healthcare provider for preventive physical therapy were 89.4% less likely to receive an opioid prescription and also had lower out-of-pocket costs.
Chiropractic care
During a chiropractic appointment, a chiropractor adjusts your body’s alignment to relieve pain. While many patients experience gradual improvements over time, the relief from pain can vary depending on the individual and their condition. Chiropractic care is often used to treat musculoskeletal-related pains, such as back and neck pain.
Like any medical treatment, chiropractic care carries some risks. Although rare, complications from spinal manipulation—particularly in the neck—have been associated with chiropractic care. However, for many individuals, the benefits of chiropractic care in managing pain and improving mobility can outweigh the risks, especially when performed by a qualified professional.
Acupuncture
Acupuncture might help treat back or neck pain, osteoarthritis, and post-operative pain. Many of the benefits last up to one year after treatment, according to the National Center for Complementary and Integrative Health (NCCIH). They also state that acupuncture may also exert a placebo effect through “nonspecific effects,” such as the patient’s belief in acupuncture as an effective treatment.
Acupuncture is generally considered safe when performed by a trained practitioner, with a low risk of adverse effects.
Massage therapy
Massage is effective for back, hand, neck, and knee pain. It may also help improve sleep and reduce anxiety and depression symptoms. According to the American Massage Therapy Association, acute pain may resolve after one or two sessions of massage therapy. However, people with chronic pain may require weekly sessions for several months or even years.
According to the American Massage Therapy Association, massage therapy is not recommended for inflamed areas because it might spread an infection or further irritate them. It is also not recommended for people with heart problems, infectious diseases, phlebitis, and certain skin conditions.
Meditation and mindfulness
Meditation and mindfulness reduce pain by redirecting attention elsewhere. Although the exact mechanism is still being investigated, they have demonstrated their effectiveness for managing chronic pain and have been shown to be superior to placebo.
Biofeedback
Employing similar techniques to meditation and mindfulness, biofeedback is a mind-body technique wherein you exert control over your heart rate, breathing pattern, and muscle movements. This approach uses electrical pads to gather subtle signals about the way your body reacts to pain, such as a slightly elevated heart rate. You are then able to recognize how your body responds to stressors and learn to relax your muscles to alleviate tension and pain.
Heat and cold therapy
Heat therapy is effective for treating acute low back pain and other forms of pain. If an injury is the cause of your pain, use ice for the first 48 to 72 hours to reduce swelling. Hot packs are great for relieving pain, but you should use them only 48 hours after suffering an injury and for no more than 10 to 15 minutes at a time. Wait about 20 minutes between treatments to avoid excessive heat or cold injuries.
Cognitive behavioral therapy (CBT)
Pain is often viewed in terms of its physical manifestations, but it also has emotional and psychological components, according to the American Psychological Association (APA). Stress may cause your muscles to tense up, which may increase pain. A psychologist can provide you with guidance to help you manage your emotions to limit chronic pain.
Rest
Rest treats pain caused by repetitive strain or overuse and injuries like muscle sprains or strains. If you know what activity caused the pain, reduce its intensity or stop it altogether, and the pain will often resolve on its own. However, when treating back pain, use bed rest sparingly, as too much may make the pain worse.
Immobilization
Immobilization typically treats acute pain associated with an identifiable cause, such as surgery or injuries like broken bones or sprains. It helps reduce inflammation and may prevent further injury. Immobilization is typically performed at the site of an injury and involves medical devices like bootwalkers or splints.
Elevation
Elevating an injured body part relieves pain by reducing inflammation. It works by causing fluids to flow away from an injured area to other parts of the body. It is also part of the RICE treatment: rest, ice, compression, and elevation.
Medication alternatives to opioids
If your pain refuses to go away or its intensity remains high even after the above techniques, medication may be necessary to prevent it from affecting your day-to-day life.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
In a review that analyzed 183 randomized controlled trials, NSAIDs appeared to be more effective than opioids for surgical dental pain and kidney stones and had the same efficacy as opioids for low back pain. Due to the anti-inflammatory mechanism, NSAIDs can be very beneficial in managing acute pain. In addition, they posed a lower risk of nausea, dizziness, and drowsiness compared to opioids. Examples of commonly prescribed NSAIDs include ibuprofen, naproxen, Celebrex, and Voltaren.
However, NSAIDs come with risks. High doses and long-term use of NSAIDs can increase the risk of serious side effects. All NSAIDs, except aspirin, can increase the risk of cardiovascular or heart problems. Additionally, NSAIDs increase your risk of gastrointestinal (GI) bleeding, as well as disrupting kidney function. Extreme caution should be used in older patients and those with a history of stomach ulcers or cardiovascular disease.
Acetaminophen
Tylenol (acetaminophen) is less effective for treating inflammatory pain but it has fewer side effects, like nausea, dizziness, and drowsiness, than NSAIDs.
Antidepressants
Antidepressants can treat chronic pain at lower doses than is needed to treat depression. They can treat a variety of pain (even in the absence of a depression diagnosis), including arthritis, diabetic neuropathy, spinal cord injury, stroke, and migraines. The low doses mean they generally have mild side effects.
Specifically, tricyclic antidepressants (TCAs) are commonly used to help manage pain. These medications include:
- Amitriptyline (Elavil)
- Clomipramine (Anafranil)
- Desipramine (Norpramin)
- Doxepin (Silenor)
- Imipramine (Tofranil)
- Nortriptyline (Pamelor)
- Protriptyline (Vivactil)
Anticonvulsants
Anticonvulsants like gabapentin and pregabalin are commonly prescribed as first-line treatments for managing neuropathic pain due to their ability to reduce the transmission of pain signals in the nervous system. Gabapentin is typically prescribed initially, followed by pregabalin if it is ineffective.
Side effects like drowsiness, dizziness, confusion, or swelling in the feet and legs may happen but are often manageable or mitigated by starting with a low dose and gradually increasing it.
Topical pain relievers
Topical pain relievers include NSAIDs and acetaminophen, as noted above. The advantage of a topical application of medicine is that it is delivered to the site of the injury rather than throughout the entire body, which may reduce side effects. Other topical pain relievers include lidocaine and capsaicin—a naturally occurring compound that treats burning or shooting nerve pain.
Topical pain relievers generally come in patches or liquid forms, such as gels, creams, or ointments.
Advanced pain treatment options
Many of the techniques discussed so far are available without medical assistance. However, more advanced treatment options may be necessary if treatment fails to ease your pain, and these options typically do require assistance from a medical professional.
Nerve blocks
Nerve blocks can treat spinal, leg, and neck pain by injecting anesthetics into the affected area. They offer both short- and long-term relief but come with risks, such as infection and nerve injury.
Spinal cord stimulation
Spinal cord stimulation uses electrical pulses near the spine to relieve chronic back pain and neuropathic conditions. It provides varying degrees of relief and can last from months to years.
Radiofrequency ablation
Radiofrequency ablation targets nerves responsible for pain in the lower neck and joints, offering long-term relief for chronic pain. Recovery is quick, and relief can last from six months to several years.
Intrathecal drug delivery
Intrathecal drug delivery is a surgical procedure in which a device is implanted to deliver medication directly to the fluid around the spinal cord. It treats chronic back, neck, and abdominal pain as well as sciatica and cancer pain.
Lifestyle changes to help with managing pain
Lifestyle habits, such as a sedentary lifestyle, unhealthy diet, or poor sleep schedule, can exacerbate pain. Making minor, long-term changes may reduce pain and improve quality of life.
Exercise
If you are living with chronic pain, consider performing low-impact exercises (to avoid further injuring yourself). Some exercises to try include:
- Walking: A simple, everyday activity that eases pain by strengthening your core and leg muscles.
- Swimming: Very low-impact because water supports your body and removes stress on your joints and spine. This makes it particularly effective for relief from back pain.
- Cycling: Especially useful for treating pain in beginners, elderly patients, and patients with joint issues.
- Yoga: Helps with chronic lower back pain by strengthening core muscles, improving flexibility, and encouraging proper posture.
Healthy diet
Chronic pain is often caused by chronic inflammation, and diet plays a key role in managing it. The Mediterranean diet is a popular anti-inflammatory diet that reduces your intake of processed foods and red meat and increases your consumption of fresh produce and healthy fats.
Joint pain may be worsened by excess weight, with as little as 10 pounds greatly increasing the load on the joints, potentially accelerating cartilage breakdown and causing chronic pain.
A healthy diet is often recommended as part of a holistic treatment plan alongside several of the other treatment options in this guide, such as exercise, physical therapy, and acupuncture.
Sleep
Sleep and pain are interrelated in that pain during the day decreases your quality of sleep, which, in turn, increases pain levels the next day. It may be difficult to break this cycle, but there is some evidence to suggest that cognitive behavioral therapy for insomnia (CBT-I) improves sleep quality and reduces pain. Other ways to improve the quality of sleep are to exercise during the day and to cut back on caffeine use.
Managing stress
When you’re stressed, your muscles tense up, which may lead to pain in your neck, shoulders, and back. Chronic stress and inflammation also contribute to pain. Many of the techniques in this guide (such as exercise and improved sleep) can help manage stress and decrease the likelihood of chronic inflammation and pain.
Complementary therapies
Complementary therapies can be a helpful addition to your pain management plan, working alongside traditional treatments to provide more relief. These approaches focus on the whole person, addressing both physical and emotional aspects of pain to support your overall well-being.
Herbal remedies
Since many FDA-approved medications are derived from plants and herbs, it’s no surprise that herbal remedies help relieve pain. Some herbal compounds help manage arthritis pain, such as turmeric, ginger, and willow bark—the latter of which contains a precursor to aspirin. You should use herbal remedies in addition to—not instead of—proper medical care.
Supplements
Some common supplements may help relieve pain, including:
- Vitamin D: a deficiency is common in patients with osteoarthritis
- Vitamin B12: a deficiency may cause tingling in the hands, legs, or feet or an inflamed tongue
Note that supplements are underregulated compared with FDA-approved medications and may contain large discrepancies in their advertised contents. You should never use supplements as replacements for medication or medical care. Additionally, some supplements may interact with the medications you take. Always ask a healthcare provider before starting a new supplement.
Aromatherapy
Some studies have suggested that aromatherapy may help with acute pain (such as postoperative pain) when combined with other treatment options. However, the evidence is less compelling for using it for acute pain, such as during labor.
Hypnotherapy
Hypnotherapy may help you deal with pain and also address contributors to pain, such as stress and anxiety. Patients often combine hypnotherapy with other treatments (such as cognitive behavioral therapy) and may use it to treat other factors contributing to stress, such as excess weight or smoking.
Patient support and education
Patient support and education play a crucial role in managing chronic pain. Connecting with others who understand your experience and gaining the right tools can help you feel more in control and improve your overall quality of life.
Support groups and counseling
The U.S. Pain Foundation hosts monthly virtual chronic pain support groups via Zoom led by support group leaders who have completed a training program to facilitate discussions among attendees.
Self-management programs
A variety of online and in-person pain self-management programs help adults build skills to manage their chronic pain.
Technology in pain management
Technology is transforming pain management by providing innovative ways to monitor and treat pain from the comfort of your home. From telemedicine to mobile apps and wearable tech, these tools can enhance traditional treatments, offering greater flexibility and personalized support for managing chronic pain.
Telemedicine and telehealth
The COVID-19 pandemic accelerated the use of telemedicine and telehealth, including for pain management. Healthcare providers can conduct behavioral interventions like stress management, modifying thoughts, and physical activity recommendations. They can also issue prescriptions if necessary. Telemedicine is suitable for monitoring postoperative, pediatric, cancer, and noncancer pain, as well as nonmedical self-management strategies.
Mobile apps for pain management
The U.S. Pain Foundation recommends several apps to help manage pain, including:
- Branch Health is an app for managing chronic pain that also provides data analysis and social support.
- Pathways Pain Relief offers guidance to understand your pain and develop strategies to deal with triggers.
- Curable offers guided meditations as well as lessons and help for creating plans to manage your pain.
Wearable tech and biofeedback devices
- RESPeRATE is an FDA-approved device effective at lowering blood pressure, which is a cause of headaches and chest pain.
- Apple Watches, when combined with specific apps, can reduce symptoms of depression, opioid use, pain severity, and disability when added to a pain management program.
- Not All Pain is Created Equal: Basic Definitions and Diagnostic Work-Up, Pain and Therapy (2020)
- NIH study finds high rates of persistent chronic pain among U.S. adults, National Institutes of Health (2023)
- Understanding the opioid overdose epidemic, Center for Disease Control (2024)
- NIH study finds high rates of persistent chronic pain among U.S. adults, National Institutes of Health (2023)
- Analysis of opioid efficacy, tolerance, addiction and dependence from cell culture to human, British Pharmacological Society (2012)
- Nonopiod therapies for pain management, Center For Disease Control (2024)
- Physical therapy, Institute for Quality and Efficiency in Health Care (2024)
- Pain relief through physical therapy, University of Utah Health (2016)
- Physical therapy as the first point of care to treat low back pain: An instrumental variables approach to estimate impact on opioid prescription, health care utilization, and costs, Health Services Research (2018)
- Chiropractic care for pain relief, Harvard Health Publishing (2021)
- Acupuncture: Effectiveness and safety, National Center for Complementary and Integrative Health (2022)
- Therapeutic massage for pain relief, Harvard Health Publishing (2016)
- Parameters of pain, American Massage Therapy Association
- Brain scans reveal that mindfulness meditation for pain is not a placebo, UC San Diego Today (2024)
- Biofeedback, Mayo Clinic (2023)
- Treatments for acute pain: A systematic review, Agency for Healthcare Research and Quality (2020)
- When to treat pain with ice vs heat, Piedmont
- Ice packs vs. warm compresses for pain, Johns Hopkins Medicine
- Managing chronic pain: How psychologists can help with pain management, American Psychological Association (2013)
- Resting for pain, Delaware Valley Pain and Spine Institute
- Bed rest for back pain? A little bit will do you, Harvard Health Publishing (2017)
- Immobilization, University of Arkansas for Medical Sciences (2024)
- Are there nonsurgical treatments for foot and ankle problems?, University of Arkansas for Medical Sciences (2024)
- How to use the R.I.C.E method for treating injuries, University of Pittsburgh Medical Center
- Antidepressants: Another weapon against chronic pain, Mayo Clinic (2019)
- Anti-seizure medications: Relief from nerve pain, Mayo Clinic (2019)
- Topical analgesics in the management of acute and chronic pain, Mayo Clinic Proceedings (2013)
- Nerve blocks, Johns Hopkins Medicine
- Spinal cord stimulation, StatPearls Publishing (2023)
- Spinal cord stimulation in pain management: A review, Korean Journal of Pain (2012)
- Radiofrequency Ablation for Pain Management, Cleveland Clinic (2022)
- Intrathecal drug delivery, UCSF Health
- 10 ways to reduce pain, National Health Service (2023)
- Swimming for pain relief, Southside Pain Specialists (2020)
- How an anti-inflammatory diet can relieve pain as you age, Cleveland Clinic (2019)
- Role of body weight in osteoarthritis, Johns Hopkins Arthritis Center (2024)
- Sleep and pain, Journal of Bone and Mineral Research Plus (2022)
- Is sleep the new treatment for pain? Two issues need resolving before deciding, Sleep (2024)
- 20 ways to relieve stress, Cleveland Clinic (2024)
- The effectiveness of aromatherapy in reducing pain: A systematic review and meta-analysis, Pain Research and Treatment (2016)
- Aromatherapy for pain management in labour, Cochrane Database of Systematic Reviews (2011)
- National chronic pain support groups, Pain Connection (2024)
- Self management, U.S. Pain Foundation
- Telehealth and chronic pain management from rapid adaptation to long-term implementation in pain medicine: A narrative review, PAIN Reports (2021)
- 10 best apps for people with chronic pain, U.S. Pain Foundation (2021)
- Branch health: Pain management App, Softonic
- Online pain management program, Pathways
- Curable app, Curable Health
- RESPeRATE
- Long-term use of wearable health technology by chronic pain patients, The Clinical Journal of Pain (2022)