Key takeaways
There is no specific research on the interaction between Humira (adalimumab) and alcohol, but combining them could theoretically increase the risk of liver damage.
Humira is used to treat various autoimmune conditions by suppressing the immune response and is part of a class of medications known as TNF blockers.
Chronic use of alcohol can lead to inflammation and liver problems, conditions that Humira aims to control, suggesting a potential negative interaction when combined.
Patients taking Humira, especially those also on other medications like methotrexate or pain relievers, should consult their healthcare provider to understand the risks of mixing it with alcohol.
Humira (adalimumab), made by AbbVie, Inc., is the number one best-selling drug according to global sales—and has been since 2012. It is an injectable prescription drug used to treat autoimmune conditions like rheumatoid arthritis, Crohn’s disease, and psoriasis. The medication is a class of biologic medications known as tumor necrosis factor (TNF) blockers.
What is a TNF blocker?
TNF is a substance in the body that can cause inflammation. Inflammation is a normal part of your body’s defense system. But, for people with certain immune conditions, excessive inflammation is harmful. Humira suppresses your immune response. It binds to TNF and prevents it from triggering the inflammatory reaction. Besides Humira, other TNF blockers include:
What is Humira used for?
Humira can be used used for:
- Rheumatoid arthritis (RA) in adults
- Juvenile idiopathic arthritis (JIA) in patients 2 years and older
- Psoriatic arthritis in adults
- Ankylosing spondylitis in adults
- Crohn’s disease in adults and children 6 years and older
- Ulcerative colitis in adults and children 5 years and older
- Plaque psoriasis in adults
- Hidradenitis suppurativa in patients 12 years and older
- Uveitis in adults and children 2 years and older
As with any medication, there are benefits and potential risks—such as interactions with food, drinks, or other medications.
RELATED: Learn about these 8 common types of arthritis
Can you mix Humira and alcohol?
There is no research on how Humira and alcohol interact in your body. However, just because alcohol and Humira have not been studied does not mean that it is safe. Chronic alcohol use can lead to inflammation—increasing the reaction that Humira is trying to suppress.
Additionally, when you take a TNF blocker, like Humira, there is a risk for developing liver problems, including long-term liver damage or even death. Alcohol can also damage your liver. In fact, liver problems from alcohol use are on the rise in the U.S.
With either Humira or alcohol use having the potential to impair this vital organ, there could theoretically be an increased risk of liver damage when the two are combined. Because any TNF blocker can cause liver problems, this increased risk could apply to other drugs in this class: Remicade, Enbrel, Cimzia, and Simponi.
If you take Humira and experience any of the following symptoms, you should call your doctor right away:
- Tiredness
- Appetite loss
- Vomiting
- Abdominal pain
- Yellowing of the skin or the whites of the eyes
These could be a sign of a liver problem. 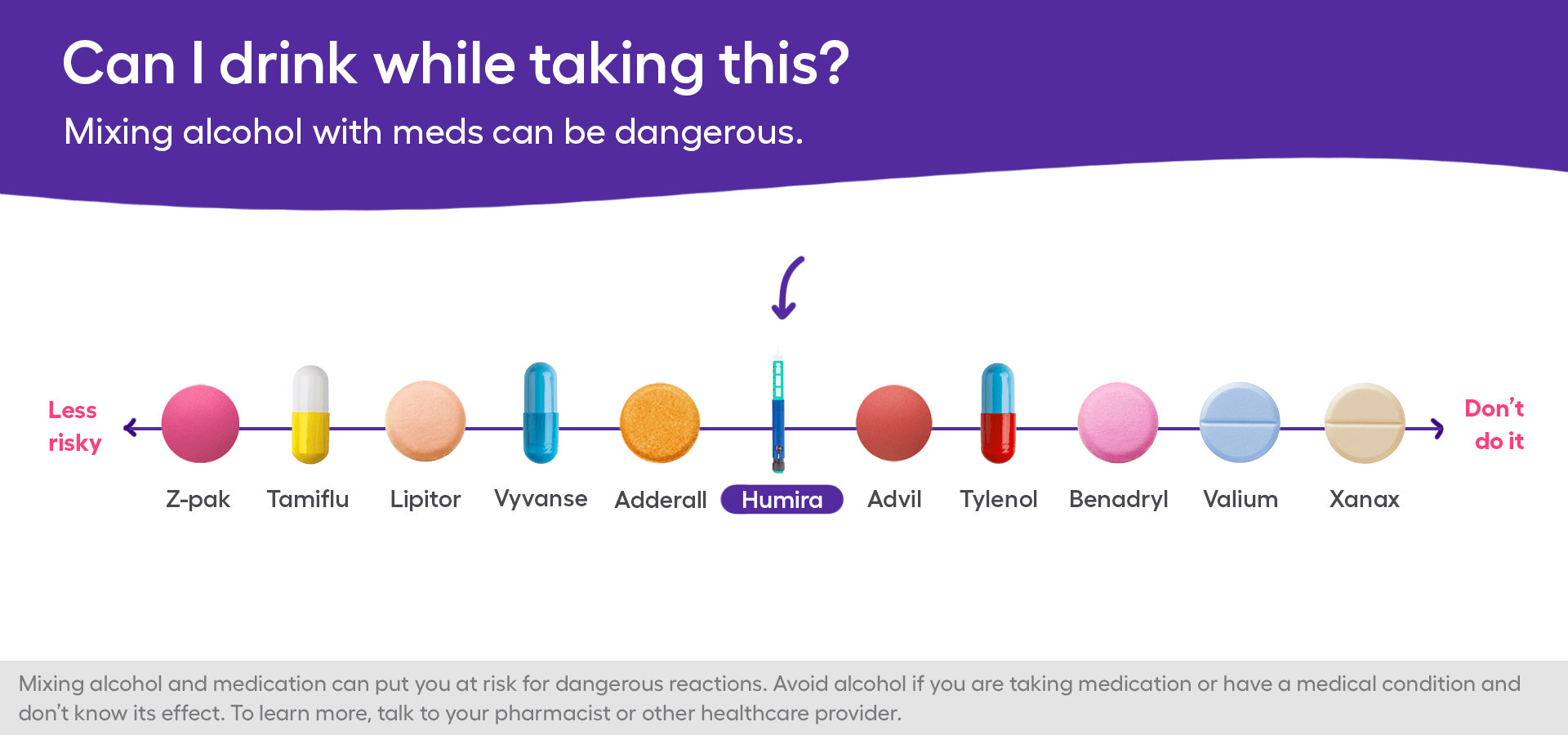
Can you mix alcohol with your other prescriptions?
People who take Humira often take other medications as well to manage their conditions. Those can also interact with alcohol or lead to liver damage.
For example, methotrexate is an Rx commonly prescribed alongside Humira for rheumatoid arthritis or psoriasis. This medication also carries the risk of liver damage, cirrhosis, and liver failure—a risk that increases with heavy drinking.
Additionally, pain relief medications—such as Tylenol (acetaminophen) and nonsteroidal anti-inflammatory drugs (NSAIDs) like Celebrex (celecoxib) or Mobic (meloxicam)—may cause liver problems or increase risk of gastrointestinal (GI) bleed when mixed with alcohol.
The bottom line
Every patient has a unique situation regarding medical conditions, history, and other medications they take. Before taking Humira, tell your healthcare provider about all of your medical conditions and any medications you take, including prescription drugs, OTC medicines, and supplements.
With this information, your physician can evaluate your individual situation and advise if (and how much) alcohol is safe for you.




