Key takeaways
Heat-related illnesses, such as heat stroke and heat cramps, can range from mild to life-threatening conditions caused by the body overheating.
The body’s temperature regulation, managed by the hypothalamus, can fail during excessive heat.
Symptoms and treatments of heat-related illnesses range from heavy sweating and fainting to muscle cramps and rashes.
The warm, sunny days of summer are here again, and with the warmth come heat-related illnesses like heat exhaustion and heat cramps. Collectively known as hyperthermia, heat-related illnesses are mostly preventable conditions that occur when your body temperature gets too high, and they can range from a mild rash to life-threatening heat stroke.
If you or your kids are going to be out in the hot sun for any extended period of time, you should know the signs of heat-related illnesses and what you can do to prevent or treat them before they become dangerous.
How does the body regulate temperature?
Most of the time, your body temperature hovers at roughly 97–99 degrees Fahrenheit (F) thanks to a part of your brain called the hypothalamus. The hypothalamus compares your current body temperature to normal body temperature, and if your current body temperature is too low, the hypothalamus directs your body to generate more heat for your internal organs. If your body temperature is too high, the hypothalamus sends signals to nerves in your skin to generate sweat to cool your skin down.
But sometimes when you get too hot, your hypothalamus just can’t keep up. When this happens, “the sweat production and evaporation process is slowed down, and your body temperature rises,” says Mary Campagnolo, MD, a family physician in Bordentown, New Jersey.
Amy Cram, MD, a pediatrician with Greenwich Hospital in Greenwich, Connecticut, adds: “You cool down by sweating and by your blood vessels dilating and releasing heat. You warm up by blood vessels constricting and preserving heat.”
A body temperature greater than 100.4 F is considered a fever. Anything greater than 103 F is considered a high fever. Hyperthermia is defined as a body temperature greater than 104 F, and during heat stroke, your body temperature can climb as high as 106 F in just 10 to 15 minutes, according to the Centers for Disease Control and Prevention (CDC).
6 heat-related illnesses
Too much exposure to heat and humidity can lead to heat-related illnesses that quickly progress from mild to severe. This is especially true if you become dehydrated, which happens when you don’t ingest adequate fluids to replace the ones you’re sweating out. Keep your eye out for these six heat-related illnesses this summer.
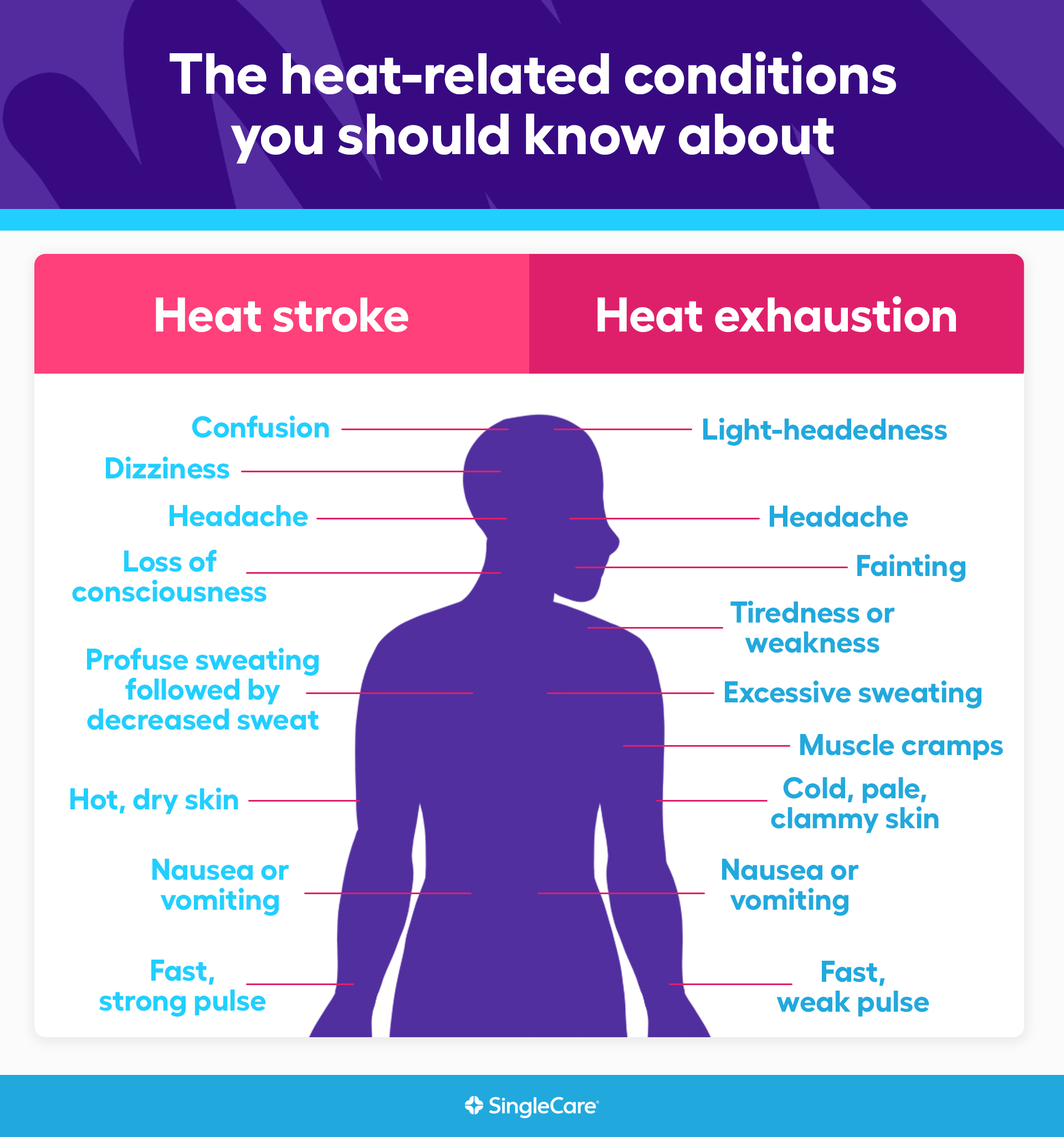
1. Heat stroke
The most serious type of heat-related illness, heat stroke occurs when your body’s ability to regulate its own temperature stops working. Your body temperature can climb past 104 F and quickly reach 106 F or more, which is too high for your brain and organs to tolerate. Heat stroke is a medical emergency that requires immediate attention. Untreated heat stroke can lead to death or permanent disability.
Heat stroke is most common in hot and humid conditions during the summer months. Older adults and young children are more susceptible to heat stroke, as are people who overexert themselves in the heat, such as athletes and military trainees. In addition to a very high fever, warning signs of heat stroke include the following:
- Confusion
- Dizziness
- Loss of consciousness
- Nausea or vomiting
- Headache
- Fast, strong pulse
- Profuse sweating followed by decreased sweat and hot, dry skin
“Heat stroke is the most severe heat-related illness, identified by flushed, red skin, decreased sweat, internal temperature greater than 104 degrees Fahrenheit, fainting, shortness of breath, and seizures,” Dr. Campagnolo says. “It can lead to cardiac arrest and death.”
Call 911 or get someone to a hospital emergency room right away if you think they might be experiencing heat stroke. First aid for heat stroke is aimed at cooling the person’s body temperature back down to a normal range as quickly as you can. Move the person to a shaded, preferably air-conditioned place, if possible, and place cool cloths on their armpits, groin, head, and other hot spots. If you can, place the person in a bath of cold water or ice to cool the person’s skin down until paramedics arrive. If the person is able to drink, give them small sips of cool water to help them rehydrate.
2. Heat exhaustion
When you’re in a hot environment and your body first starts to overheat, you may sweat heavily or have an elevated heart rate. These could be signs of heat exhaustion, a preventable illness that can progress to heat stroke if steps aren’t taken to cool your body down.
Older adults and young children are at higher risk of heat exhaustion. Symptoms of heat exhaustion include:
- Excessive sweating
- Fast, weak pulse
- Nausea or vomiting
- Muscle cramps
- Cold, pale, clammy skin
- Headache
- Tiredness or weakness
- Light-headedness
- Fainting
If you suspect someone is experiencing heat exhaustion that might become heat stroke, seek medical attention right away. Otherwise, in most cases, you can treat heat exhaustion on your own.
“The first step is to get the affected person into a cooler environment, whether in a shady area or indoors with air conditioning, if possible,” says Campagnolo. Once the person is in a cool place, give them a damp cloth to hold on their forehead, and have them drink cold drinks to stay hydrated. Avoid caffeinated, sugary drinks and stick to cool water or sports drinks, which contain electrolytes like the ones lost in the sweating process. If necessary, have the person soak in a bath of cold water or ice. If these measures aren’t enough to make the person feel better after an hour, seek medical care.
3. Rhabdomyolysis
Also known as rhabdo, rhabdomyolysis is a rare illness that occurs when muscle fibers break down or die rapidly and leak a protein called myoglobin into the body’s circulatory system. Myoglobin is normally filtered out of the blood by the kidneys, but too much myoglobin can lead to kidney damage, kidney failure, and death. Rhabdo is included as a heat-related illness because heat stress and dehydration from hot conditions or physical activity can lead to muscle breakdown.
Firefighters and endurance athletes are among those who have a higher risk of rhabdo. Symptoms of rhabdomyolysis, which can range from mild to severe, include:
- Muscle pain and tenderness
- Muscle swelling or bruising
- Weakness
- Fever
- Nausea or vomiting
- Dark or tea-colored urine
- Confusion or delirium
- Loss of consciousness
Rhabdomyolysis is an emergency situation that requires immediate medical attention. If you think someone has rhabdo, call 911 or get them to a hospital emergency room right away. In the meantime, get the person to move to a cool area, stop all activity, and drink extra fluids to stave off dehydration, which can make rhabdomyolysis worse.
4. Heat syncope
A relatively mild form of heat-related illness, heat syncope is a fainting episode that often results in hot or humid conditions due to physical exertion, prolonged standing, or getting up quickly from a seated or lying position. The heat and other conditions cause a drop in blood pressure flowing to the brain, which causes you to faint.
Dehydration or not being acclimated to the conditions or elevation can make heat syncope more likely. In addition to a brief loss of consciousness (syncope), symptoms of heat syncope can include:
- Dizziness or light-headedness
- Headache
- Increased heart rate
- Nausea or vomiting
To treat heat syncope, have the person lie or sit down in a cool area, elevate their feet, and drink water or sports drinks. They should also take a break from any exertional activities until they’ve had a chance to rehydrate and their symptoms are gone.
5. Heat cramps
These painful, involuntary muscle spasms usually affect athletes and workers who sweat a lot in hot, humid conditions. The sweat drains your body of salt and moisture, both of which your muscles need to function properly. Low salt levels in your muscles causes them to cramp up. Heat cramps and heavy sweating can also be signs of heat exhaustion.
To treat heat cramps, move to a cool area, drink water or sports drinks, and stop any strenuous activity until long after the cramps have stopped. Gently stretch and massage the affected muscles—most often the muscles of the arms, calves, back, or abdomen—to help make the cramps stop. If the muscle cramps don’t go away within an hour, call a healthcare provider.
6. Heat rash
Sometimes called prickly heat or miliaria, heat rash is a skin rash that develops in hot and humid conditions when your pores become blocked and sweat can’t escape. The resulting rash can be bumpy, red, or itchy and can range from mild to severe.
Heat rash is often caused by friction on your skin, which is why adults most often develop heat rash in places like their inner thighs and armpits, where skin rubs together. Babies tend to get heat rash more on their necks and in skin creases such as the ones at their elbows, thighs, and armpits. The symptoms of the rash will depend on which type of heat rash it is.
- Miliaria crystallina, the most common and mildest form of heat rash, causes small clear or white bumps that are filled with fluid and often burst open.
- Miliaria rubra, or prickly heat, occurs deeper in the skin and causes red bumps and itching or a prickly sensation in the affected area.
- Miliaria pustulosa occurs when the red blisters, or vesicles, of miliaria rubra become inflamed and filled with pus.
- Miliaria profunda, the least common kind of heat rash, occurs deep in the skin when retained sweat leaks out of the sweat gland and into the skin, causing larger, firm, flesh-colored bumps.
In some cases, miliaria profunda can recur often and become chronic, but other than that, most cases of heat rash will go away on their own in a few days. To treat heat rash, stay in a cool, dry place, avoid sweating or exertion, and use baby powder rather than any creams or lotions to soothe the rash.
What can cause heat intolerance?
Extreme heat and high humidity are the most obvious causes of heat-related illnesses, but what causes some people to be more susceptible to heat stress than others? Infants and children younger than 4 are at higher risk because a child’s body’s ability to regulate its own temperature hasn’t fully developed yet. Adults 60 and older may also be at higher risk because their ability to regulate their body temperature may be diminished by age, illnesses, or the medications they may be taking to treat other medical conditions. Medications that can affect the body’s ability to stay hydrated and respond to heat include beta blockers and diuretics taken to treat high blood pressure and heart problems, antihistamines taken for allergy symptoms, tranquilizers, and antipsychotics used to treat psychiatric symptoms.
People who are overweight or obese typically have more problems with hot weather and humid environments than people of a healthy weight. Others who may be more susceptible to heat exhaustion and heat stroke include people who work or play in hot conditions. This includes athletes, firefighters, military personnel, farm workers, and others who have to spend many hours in the sun. And anyone subjected to a sudden temperature change—for example, someone flying in January from Minnesota to Florida—may have a harder time dealing with the heat until they become acclimated.
Heat illness prevention tips
If you or your kids will be going out in the sun, you probably already know that you should use a high-SPF sunscreen to avoid sunburn. The CDC recommends an SPF rating of 15 or higher, but no amount of SPF will help you with high temperatures and heat exposure. To prevent heat-related illnesses, limit your time in the heat, drink plenty of fluids to avoid dehydration, and wear loose-fitting, lightweight clothes.
If you’re taking any medications or you have other underlying medical conditions, take extra precautions when doing any activities in hot weather. If you have to exert yourself, try to do it early in the morning or at night, when the conditions are coolest. If you’ll be going somewhere with hotter weather than you’re used to, take the time to get acclimated before you exert yourself very much, and never, ever leave a child or pet in a parked car. This is a common cause of heat stroke in children.
If you have to work in hot conditions, “try to take breaks in the shade or in an air-conditioned environment,” Dr. Campagnolo says. “And watch your urine color. If it’s dark and concentrated, you need to drink more water. If it’s lighter and pale, you’re probably getting enough water.”
When it’s hot, “drink water, and don’t overexert,” Dr. Cram adds. “Take breaks. Slow down your work or exercise, and stay in the shade as much as possible.” And if you start to display any of the symptoms of heat-related illness, stop what you’re doing, have a cold drink, and take a little time to cool things down.
- Cooling techniques for hyperthermia, StatPearls (2022)
- Heat-related illnesses, Centers for Disease Control and Prevention (2024)