Key takeaways
Mixing clindamycin and alcohol in moderation is generally considered low-risk, but heavy drinking should be avoided due to potential worsened side effects.
Clindamycin is processed in the liver, and while rare, it can cause liver damage; heavy drinkers may face increased risks of liver problems during treatment.
Side effects of both clindamycin and alcohol may overlap, such as nausea, vomiting, upset stomach, and diarrhea, potentially worsening these symptoms when combined.
Although drinking in moderation while on clindamycin is unlikely to cause serious issues, consulting a healthcare provider is advised, especially for those taking other medications or with existing health conditions.
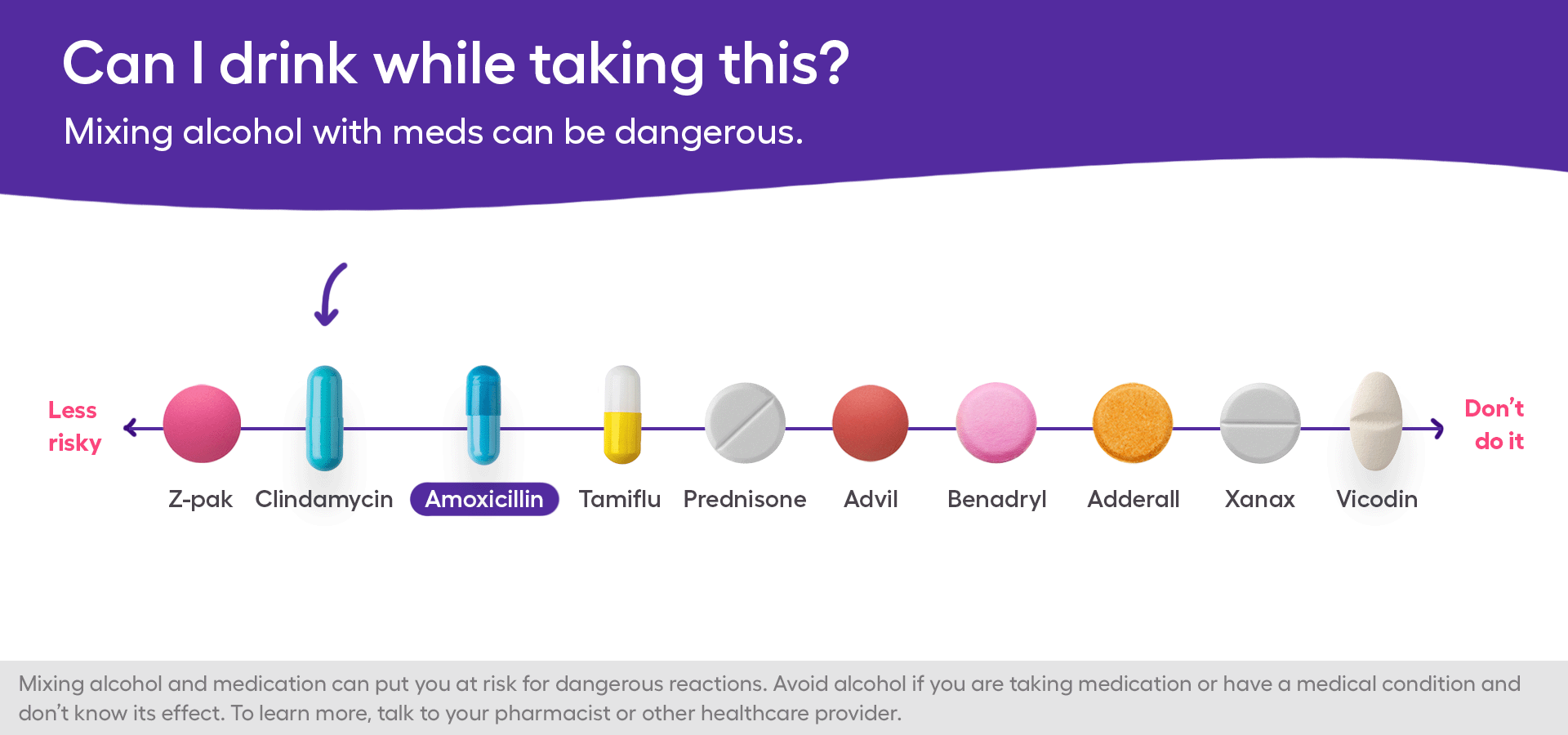
Alcohol can interact with many antibiotics, which can sometimes lead to serious side effects. However, some antibiotics, such as clindamycin, may be safer than others when mixed with alcohol. It’s unlikely that you’ll experience any severe problems while mixing clindamycin and alcohol, as long as you’re drinking in moderation.
According to the drug’s FDA label, there is no known clindamycin and alcohol interaction. Even so, the side effects of clindamycin and alcohol may overlap, so it’s best to use caution. If you’re planning on drinking on clindamycin, you may want to check with a healthcare provider beforehand, especially if you’re taking other antibiotics or medications.
Continue reading to learn more about mixing clindamycin and alcohol, the potential effects, and whether it’s safe to drink alcohol with antibiotics in general.
What is clindamycin?
Clindamycin, known by brand names such as Cleocin and Cleocin T, is a commonly prescribed antibiotic that can treat various bacterial infections. It can be prescribed to treat respiratory tract infections, blood infections (septicemia), vaginal infections, bone and joint infections, and skin infections. Clindamycin is often used to treat acne and bacterial vaginosis. It may also be prescribed for infections in people who have a penicillin allergy.
Clindamycin belongs to a group of antibiotics called lincosamide antibiotics. It is derived from lincomycin, a similar antibiotic, and it works by stopping bacterial growth or directly killing the bacteria. Different formulations of clindamycin are available, depending on the infection being treated. It can be administered as an oral capsule, injectable solution, or topical foam, gel, cream, or lotion. For acne and vaginal infections, topical clindamycin is an effective option.
Treatment with clindamycin
The dosage of clindamycin will vary based on the infection and formulation used. The usual oral dosage for adults is 150 to 300 mg every six hours. Clindamycin is usually prescribed for three to 14 days or longer, depending on the infection. In many cases, clindamycin may be combined with another antibiotic, such as gentamicin. For acne, clindamycin is often combined with other medications, such as benzoyl peroxide or tretinoin.
This antibiotic should only be used for infections caused by susceptible bacteria, including certain gram-positive and anaerobic bacteria. It is not effective for viral, fungal, or parasitic infections.
Can you drink while taking clindamycin?
There is no official warning to avoid clindamycin with alcohol. Drinking alcohol in moderation during treatment with clindamycin is unlikely to cause serious problems. Moderate alcohol use means no more than one drink per day for women and two drinks per day for men.
The risk of an interaction between clindamycin and alcohol may vary depending on the dosage form used. For instance, only about 5% of topical clindamycin is absorbed into the bloodstream. As a result, topical clindamycin is less likely than oral clindamycin to cause systemic side effects that may overlap with alcohol.
If you have questions or concerns about using clindamycin while drinking alcohol, consult a doctor or healthcare professional. They can offer medical advice on the best course of action, especially if you have other medical conditions or take other medications.
Mixing clindamycin and alcohol
As mentioned, mixing clindamycin and alcohol should generally be low-risk. However, the risk of serious effects may be increased with higher doses of clindamycin or large amounts of alcohol. Therefore, it’s best to keep alcohol intake to a minimum until you know how clindamycin affects you. You definitely will want to avoid a night of binge drinking while on clindamycin. If you drink alcohol, you may feel worse as your body fights the infection.
Alcohol does not directly interfere with how clindamycin works. However, alcohol and clindamycin may have overlapping side effects. You may experience worsened side effects of clindamycin while drinking alcohol and vice versa. Examples of worsened side effects from topical clindamycin and alcohol use may include:
- Dry skin
- Flushing or redness of the skin
- Itching or hives
These adverse effects may be more pronounced in someone who has an alcohol intolerance.
Examples of worsened side effects from oral clindamycin and alcohol consumption include:
- Nausea
- Vomiting
- Upset stomach
- Diarrhea
Side effects of clindamycin may be worsened after drinking large amounts of alcohol, as these side effects are common with alcohol intoxication. Chronic alcohol consumption is also linked to gastrointestinal side effects, such as an increased risk of ulcers, which may also occur with clindamycin.
In severe cases, clindamycin can lead to inflammation of the large intestine (pseudomembranous colitis) caused by an overgrowth of the bacteria Clostridium difficile. Symptoms of this condition include severe, watery, or bloody diarrhea, stomach pain, and fever. Alcohol can also damage the gut and lead to inflammation, especially in large amounts over time. People who chronically drink large amounts may be at a higher risk of worsened colitis and diarrhea, which can overlap with colitis caused by clindamycin.
Clindamycin, alcohol, and the liver
Clindamycin is mainly processed in the liver. In rare cases, treatment with clindamycin has been reported to cause liver damage. Specifically, jaundice and changes in liver function tests have been reported with clindamycin use. Although liver injury is typically mild, severe cases have occurred with signs of severe skin reactions. However, liver problems usually resolve within a few weeks.
People who drink heavily on a regular basis have an increased risk of alcoholic liver disease. Because of clindamycin’s potential effects on the liver, people with alcoholic liver disease may experience worsened liver problems during treatment with clindamycin.
Clindamycin, alcohol, and the kidneys
The use of clindamycin has been linked to acute kidney injury. People with kidney problems may need to use clindamycin with caution. Signs of kidney injury may include fluid retention, high blood pressure, and decreased urination. Gentamicin, another antibiotic sometimes prescribed with clindamycin, can also cause kidney injury in high doses.
Heavy alcohol consumption can lead to kidney problems, which can lead to other health problems, including electrolyte imbalances and high blood pressure. As alcohol and clindamycin may disrupt the function of the kidneys, people with preexisting kidney problems should use caution while drinking on clindamycin.
Is it safe to mix other antibiotics with alcohol?
Certain antibiotics have a higher risk of adverse effects with alcohol than others. There are known drug interactions between alcohol and tinidazole or metronidazole, for example. Drinking alcohol while taking metronidazole can cause adverse reaction symptoms, including nausea, flushing, dizziness, palpitations, increased heart rate, and shortness of breath.
Some antibiotics may cause serious gastrointestinal side effects, heart problems, or blood pressure changes. Drinking alcohol with the following antibiotics may lead to adverse reactions:
- Bactrim (sulfamethoxazole and trimethoprim)
- Zyvox (linezolid)
- Erythrocin (erythromycin)
- Cefotan (cefotetan)
- Seromycin (cycloserine)
- Gris-Peg (griseofulvin)
- Isoniazid
Due to the potential risks of mixing alcohol and antibiotics, it’s best to avoid drinking alcohol during antibiotic treatment. Drinking alcohol may also indirectly affect treatment if, for example, you forget to take a dose because you’re impaired. A missed dose could increase the risk of antibiotic resistance, leading to a worsened infection and the need for stronger antibiotics or other treatments.
Bottom line
While the risk of a serious reaction when taking clindamycin and drinking alcohol in moderation is low, other drug interactions are possible. Tell your doctor or healthcare provider about any medications you take, including prescription drugs, over-the-counter medicines, and herbal supplements, before starting treatment with clindamycin. You should also tell your doctor if you’ve had an allergic reaction to clindamycin or other antibiotics before starting treatment.
To be on the safe side, it’s usually a good idea to avoid drinking while taking antibiotics. Drinking alcohol can disrupt sleep and weaken the immune system. By avoiding alcohol, you’ll be adequately rested, and your immune system will be in the best condition to fight the infection. Still, those who drink in moderation are less likely to experience problems during treatment with clindamycin than people who drink heavily and frequently.