Key takeaways
Drinking alcohol while on blood thinners increases bleeding risks, and experts recommend avoiding the combination.
Regardless of the type of anticoagulant medication being taken, mixing it with alcohol is unsafe, impacting all common blood thinners like Coumadin (warfarin), Eliquis, Lovenox, Xarelto, Pradaxa, Savaysa, and Arixtra.
Symptoms of abnormal bleeding due to mixing alcohol with blood thinners include uncontrolled nosebleeds, dark or bright red stool, excessive bruising, and severe fatigue, among others, which can be life-threatening.
Moderate and sporadic alcohol consumption may be permissible for some individuals on blood thinners. Patients should check with a healthcare provider regarding alcohol use while on blood thinners.
If you are taking an anticoagulant, otherwise known as a blood thinner—for stroke prevention, atrial fibrillation, deep vein thrombosis, pulmonary embolism, or one of the numerous other medical conditions that, by nature, can cause blood clots—you are probably aware of the fact that these medications increase your risk of bleeding. What else thins your blood and increases your risk of bleeding? Drinking alcohol.
Put the two together and the bleeding risk increases even more, says Dr. Holly Alvarado, Pharm.D., a clinical pharmacist at Duke Health who previously worked as an anticoagulation pharmacy specialist in a cardiology clinic.
Can I drink alcohol while taking blood thinners?
“In general, I would say that [drinking while taking anticoagulants] is a bad idea,” Dr. Alvarado says. “I would recommend that people abstain.”
To make matters even worse, the metabolic changes that occur in the liver while drinking can significantly alter the effectiveness of the blood thinners, says John Beckner, R.Ph., senior director of strategic initiatives for the National Community Pharmacists Association.
“It can make the medication less effective, or it could increase that particular mechanism of action and have the opposite effect (e.g., even heavier bleeding),” Beckner says, adding that the result depends on the individual.
Want the best price on eliquis?
Sign up for eliquis price alerts and find out when the price changes!
Can I mix any blood thinners and alcohol?
Okay, but can you switch medications to make it safer to imbibe? After all, there are numerous blood thinners on the market.
Unfortunately, no—it doesn’t matter which anticoagulant you take. The warning applies to the entire class of drugs, including:
- Coumadin (many patients take warfarin, the generic version)
- Eliquis (apixaban)
- Lovenox (enoxaparin)
- Xarelto (rivaroxaban)
- Pradaxa (dabigatran)
- Savaysa (edoxaban)
- Arixtra (fondaparinux)
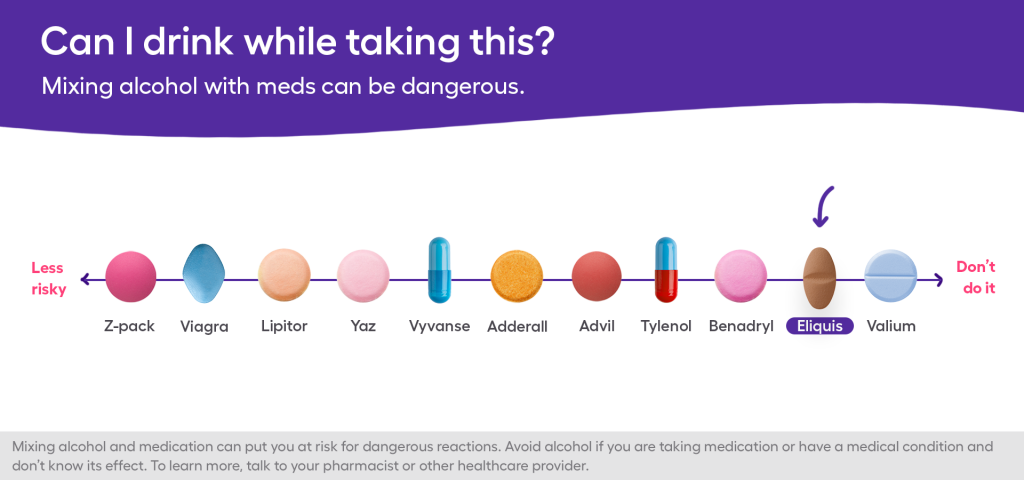
With that said, clinical trials have demonstrated that the bleeding risk associated with newer anticoagulant agents, like Eliquis, is less severe than the risk associated with others, such as Coumadin, says Dr. Alvarado. (Eliquis received FDA approval in 2012; its generic counterparts were approved late last year.) However, that doesn’t give the Eliquis and alcohol combo a pass—it is still dangerous, Beckner and Dr. Alvarado emphasize (as are all the others).
Side effects of mixing alcohol and blood thinners
Whether you are drinking or not (hopefully not, for your safety) while taking anticoagulants, be on the lookout for signs of abnormal bleeding. Seek medical attention if you experience:
- Nose bleeds, especially uncontrollable ones
- Upper GI bleeds, indicated by dark/tarry stool
- Lower GI bleeds, indicated by bright red blood in the stool
- Cuts and scrapes that won’t stop bleeding
- Bleeding gums
- Excessive/unusual bruising
- Severe fatigue
- Headache, dizziness, or confusion after a fall (especially if you hit your head)
- Vomit that is bloody or looks like coffee grounds
In some cases—if you experience bleeding gums or bruising, for example—you can simply call your doctor. Other times, an immediate trip to the ER or a call to 911 is imperative, says Dr. Alvarado, because some bleeding episodes can be life-threatening.
“If a patient fell and hit their head, they could be experiencing intracranial bleeding and not even realize it,” she says. “And by the time they are like ‘I don’t feel right,’ it might be [too late] to control it.”
So, I can never drink again?
Though Beckner and Dr. Alvarado strongly encourage their patients taking anticoagulants to abstain from alcohol altogether, they do agree that moderate, sporadic use could be okay for certain individuals. But what exactly does “moderate” mean? Well, while the National Institute on Alcohol Abuse and Alcoholism defines it as one drink a day for women and two drinks a day for men, that amount would be considered excessive and unsafe for a person taking a blood thinner. The key word here is sporadic. In other words, now and then on a special occasion.
“If I had a patient who was like ‘my daughter is getting married and I want to participate in a toast,’ I would say it is probably alright if you have one glass,” says Dr. Alvarado. “But I think it is important for patients who have even one glass to just be aware of the warning signs and to [know] what they are getting into.”




