Key takeaways
Proper medication management is crucial for people with dementia, including creating a comprehensive list of medications to identify potential drug interactions and to communicate effectively with healthcare providers.
Safe storage and organization of medications help prevent people with dementia from taking incorrect dosages or mixing up pills, with measures becoming stricter as the disease progresses.
Utilizing daily usage reminders and automatic pill dispensers can aid in ensuring medications are taken at the correct times, especially important on hectic days or as the person’s ability to remember diminishes.
Understanding drug labels and being aware of common medication issues specific to dementia, such as dangerous drug interactions and side effects, is essential for managing the health and safety of individuals with dementia.
Proper medication management is critical for people living with dementia, and it only becomes more important as the disease progresses.
Many people living with dementia are able to keep track of their medications on their own or with a little bit of help. But as the disease progresses, those with dementia may start to forget to take their pills or refuse to take them.
Also, the wrong combination of certain drugs may put dementia patients at risk of impaired cognition, fall-related injuries, and even death. One recent study found that approximately one in seven dementia patients were prescribed dangerous combinations of drugs.
Tips for effective dementia medication management
Here are the fundamentals of successful medication management and how they apply to people living with dementia.
Medication list
The first step is to fully account for every medication being taken by the person with dementia. Create a list that includes prescription drugs, over-the-counter drugs, and any herbal or nutritional supplements.
A medication list serves three purposes: it allows a patient or caregiver to see all the medications the person is taking at a glance; it provides a place to note any medication issues or side effects so that you can talk about them with his or her provider; and, it shows a doctor or pharmacist the full range of medications, so they can spot potential drug interactions.
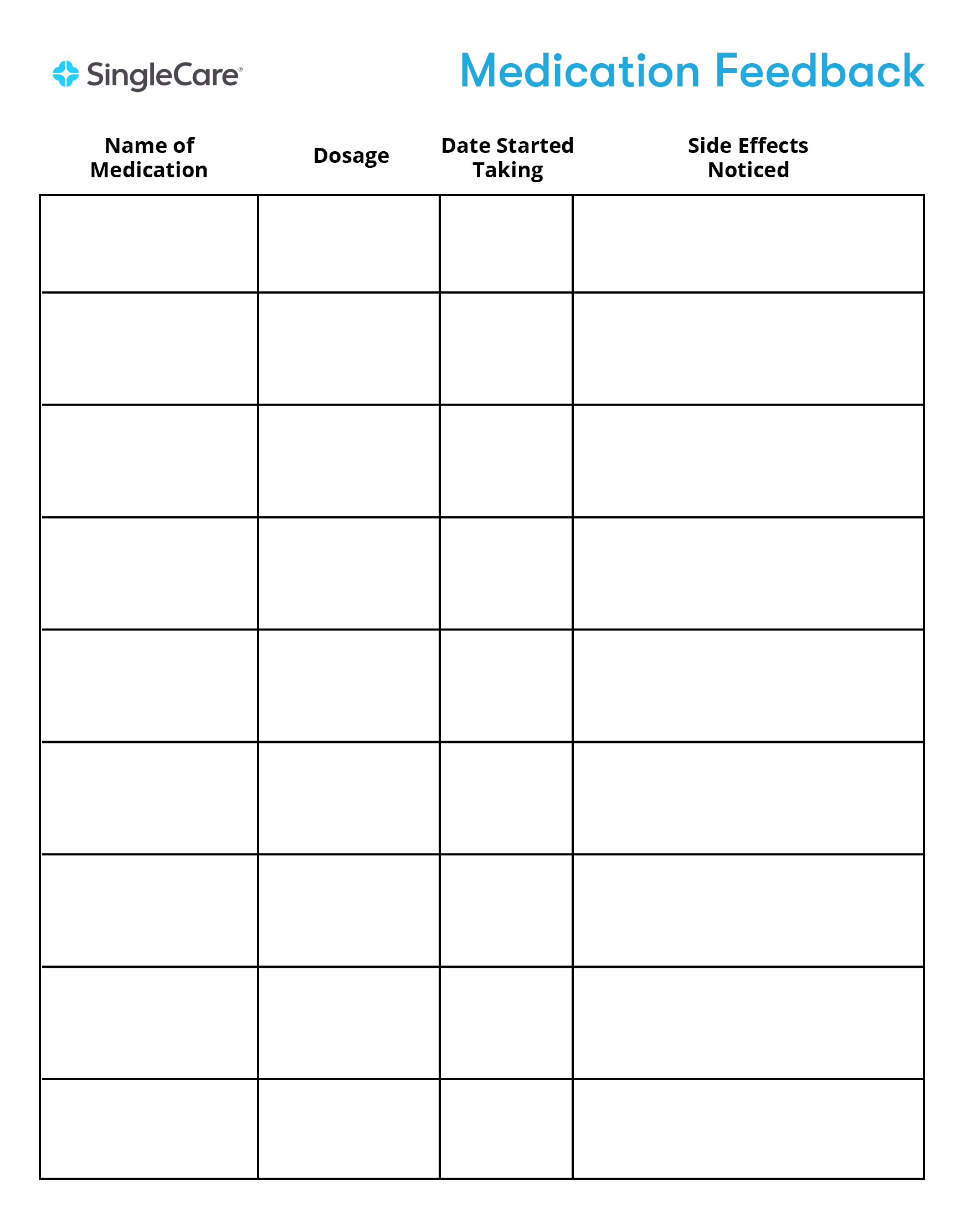
A good medication list will include the following:
- Name of each medication
- Dosage of each medication
- Dates the person started taking each medication
- An area to note side effects or other issues
We’ve created a template to help.
When filling out your medication list, it’s a good idea to start with supplements first. Supplements can be the easiest to forget since they are often considered herbal or natural—but they can still interact with prescription medications, so your doctor and pharmacist should know about these.
Next, list any over-the-counter medications that you take regularly. These could include pain relievers, allergy medications, sleep aids, and digestive medicines. While there’s nothing wrong with taking over-the-counter medications, your doctor should know if you are taking them. If there’s a risk of drug interactions, your doctor or pharmacist can recommend a different drug.
Finally, add the names of all prescription medications. Saving the original pill bottles, boxes, and containers can be a big help when you update your medication list since all the information will be right there for you to copy down. A shoebox-size plastic box or a gallon-size sealable plastic bag should have plenty of room for storing labels, bottles, and containers.
Once you’ve finished the list, run it by your healthcare provider to make sure you haven’t missed anything.
Safe storage and organization
People with dementia can often forget to take their pills. They can also forget that they have already taken their pills, which could lead to them taking a double dose. Sometimes, people with dementia can mix up pills, take incorrect dosages, or ingest the wrong medications. Proper organization and storage of medication can help prevent these incidents.
If the care team agrees that the person living with dementia is still able to manage their medication regimen, you may not have to take extreme measures to safekeep medications (unless you live with children or pets). In that case, the person living with dementia can have full access to their medication, so they can take what they need at the necessary time. This lessens the burden on caretakers since they won’t have to be present to administer every medication.
However, as the disease begins to affect the person’s cognition, lax storage habits could become dangerous. It is wise to put strict storage measures in place before a potentially dangerous accident happens. If disease progression is severe, you may need to limit the person’s access to medication altogether.
The safest storage place is usually a locked box or cabinet that can only be accessed by the caretaker. You may need a second lockbox for medications that have to be refrigerated.
Daily usage reminders
You or your caretaker may not feel you need a reminder to take or administer pills a few times a day. But consider those hectic days (like when you have plumbing problems or an appointment at an unfamiliar location) when it can be easy to forget medication schedules.
There are many different ways to create medication reminders. Use the one that makes sense for your lifestyle.
Here are some potential options for usage reminders.
- Pill reminder app: If you use your smartphone frequently, you can download one of the many pill reminder apps. They will guide you through the alarm-setting process.
- Set an alarm: Set alarms for the appropriate times on your phone, tablet, or computer.
- Make a list: Write down the medicines and times to take them, and keep the list in a prominent place.
- Add it to your calendar or planner: Add your medication information to calendars or planners, if you use them.
- Use sticky notes, send yourself emails, or post other reminders: Think about how you manage your time and how you use reminders. Choose a method that works best for you.
Timed or automatic pill dispenser
Automatic pill dispensers provide a compelling combination of secure storage and timely reminders.
The pills are preloaded into the dispenser and programmed to be delivered at the correct time. When the pill is dispensed, an alarm sounds.
Automatic pill dispensers for home use can be purchased for less than $100. The drawback of the automatic dispenser is that someone must invest the time to fill and program the machine.
Understanding drug labels
All prescription and over-the-counter drugs are sold in packaging with government-approved labels.
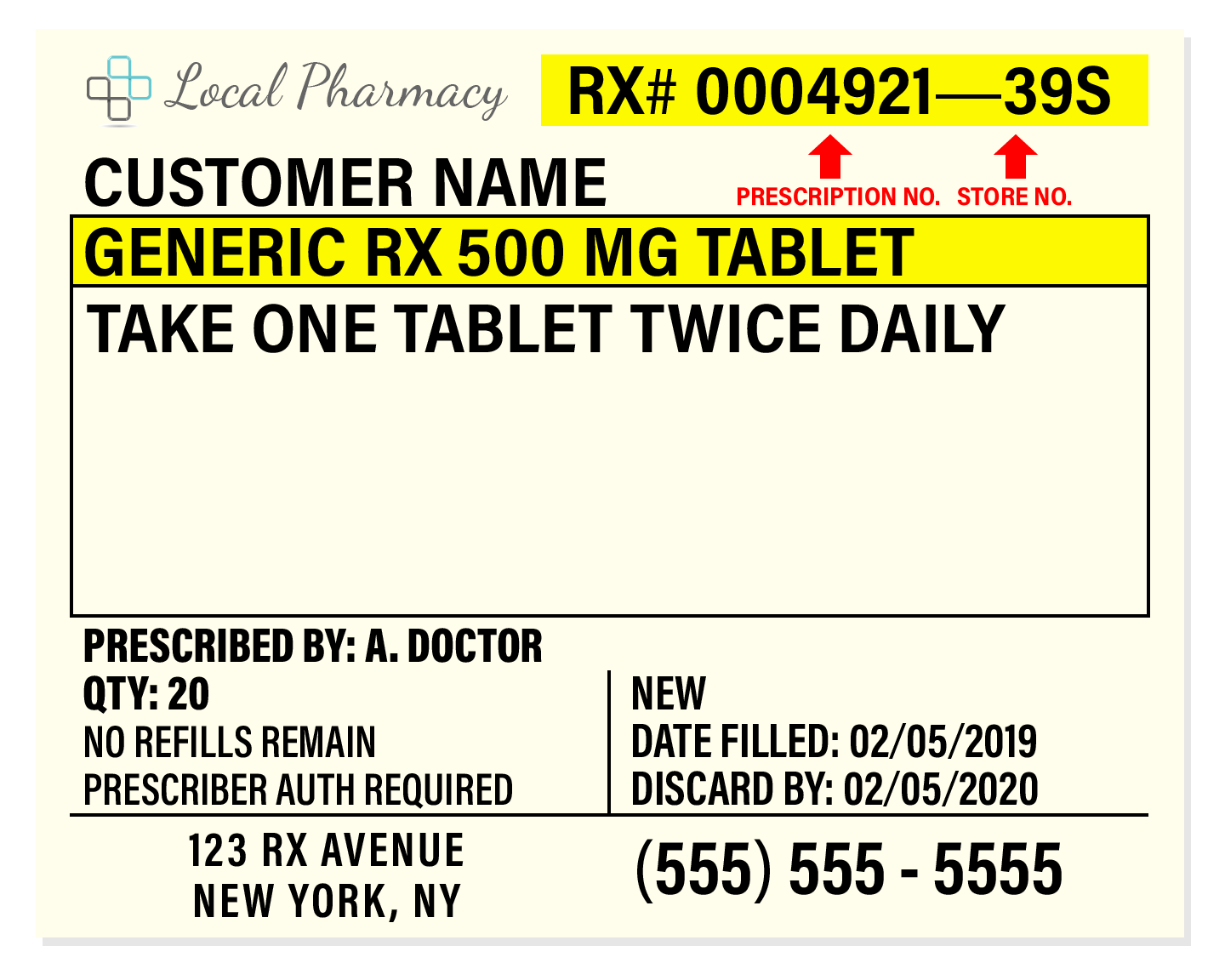
Prescription medication labels
Prescription medication labels focus on the most important information for the patient: the dosage of the medicine and how often to take it.
The rest of the information on the label is mainly for your pharmacist or other medical professional.
Here is a sample of a prescription medication label.
Over-the-counter medication “Drug Facts” label
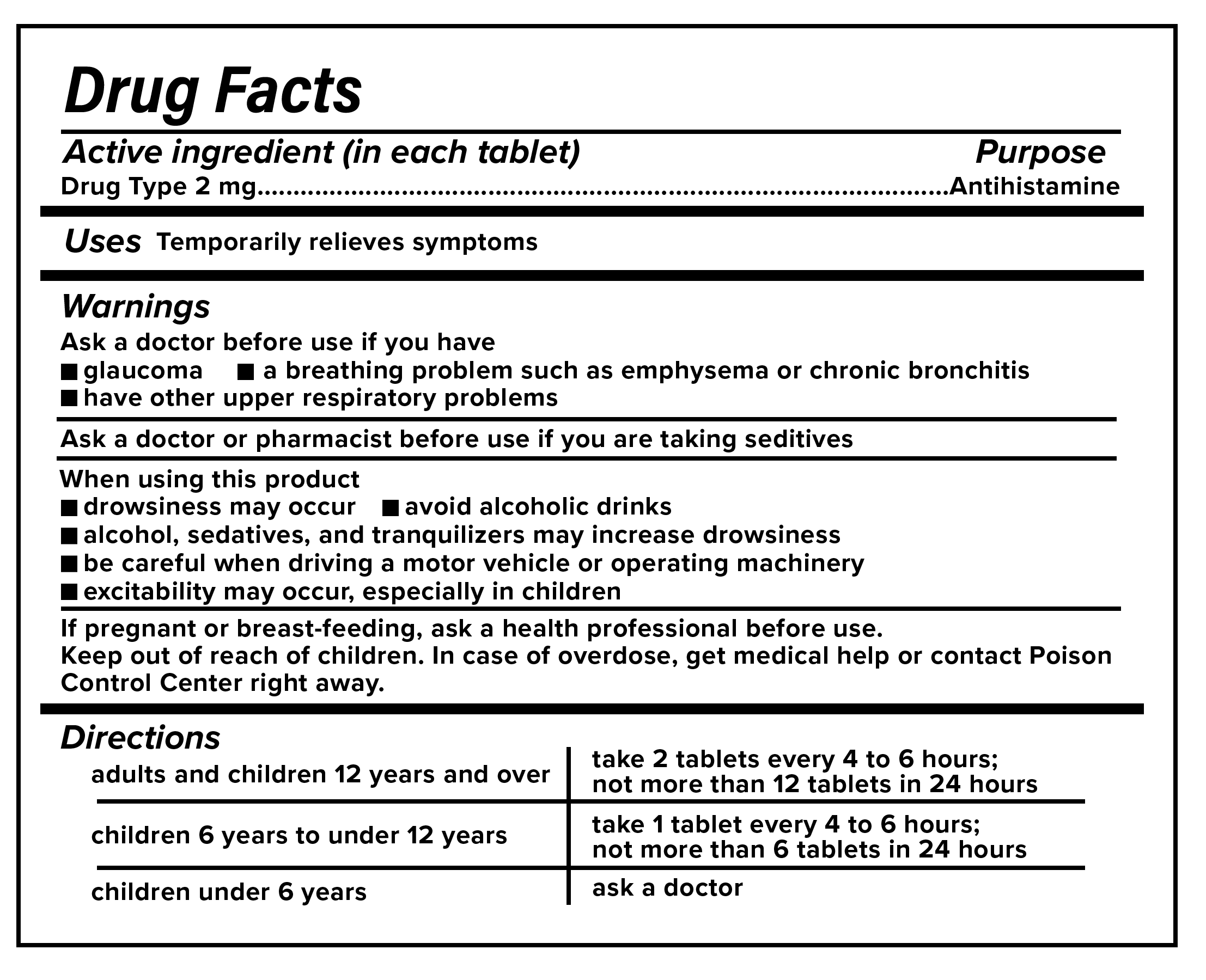
Over-the-counter medications, such as drugs to relieve cold and flu symptoms, come with a different label that has more information for the consumer. Because these medications can be purchased and taken without the supervision of a doctor, it is critical for people with dementia and their caretakers to carefully review these labels. The labels may indicate if they are inappropriate for people with certain conditions or for people taking certain drugs.
Even though the “Drug Facts” label has a lot of useful information, people living with dementia and their caregivers should always consult their doctor or pharmacist before taking a new medication or supplement.
Dangerous drug interactions
A 2015 study published in the journal of Clinical Interventions in Aging found that elderly populations are particularly at an increased risk of adverse drug reactions. This is especially true for people living with dementia because of the wide variety of drugs prescribed to them. People living with dementia may be prescribed cognitive enhancers, antipsychotic drugs, or antidepressants. Some of these medications may cause dangerous interactions if taken in combination with other medications commonly prescribed to elderly patients.
Drug interactions can lead to adverse effects that can then lead to the addition of more medications to treat the adverse effects. As the authors of the study point out: “The inability to distinguish drug-induced symptoms from a definitive medical diagnosis often results in addition of yet another drug to treat the symptoms, which in turn increases drug interactions.”
One important step you can take to minimize the risk of dangerous drug interactions is to communicate with your healthcare providers about any new or discontinued medications. You should also try to work with a single pharmacist and pharmacy so that you’re getting all your medications from one place. Getting prescriptions from fewer doctors, communicating with healthcare providers, and purchasing medications from one pharmacy can decrease the likelihood of a drug interaction.
Common medication issues specific to dementia
Doctors often prescribe powerful medications to people with dementia to try to manage or slow the progression of disease symptoms.
The Alzheimer’s Association is a non-profit organization that provides information on some of the most commonly prescribed dementia medications and their side effects.
Listed below are common side effects associated with the most commonly prescribed dementia medications. Important note: The side effects listed below are known to be common side effects. However, this is not a complete list of all possible side effects of each medication.
Side effects of drugs used to treat cognitive symptoms
These medications, which are classified as cholinesterase inhibitors, glutamate regulators, or a combination of both types of drugs, are prescribed to help boost memory and thinking.
- Aricept (donepezil): Diarrhea, loss of appetite, muscle cramps, nausea, sleep changes
- Belsomra (suvorexant): Sleepiness or unusual drowsiness, headache
- Exelon (rivastigmine): Nausea, vomiting, diarrhea, decrease in appetite
- Namenda (memantine): Constipation, diarrhea, vomiting, confusion, dizziness, headache
- Namzaric (donepezil and memantine): Headache, diarrhea, dizziness, insomnia, loss of appetite
- Razadyne (galantamine): Dizziness, headache, diarrhea, nausea, vomiting, decrease in appetite
Side effects of drugs used to treat low mood and irritability
These medications, which are antidepressants, are prescribed to help improve mood and decrease irritability.
- Celexa (citalopram): Headache, constipation, nausea, diarrhea, dizziness, drowsiness
- Paxil (paroxetine): Constipation, dizziness, headache, drowsiness, nausea, loss of appetite
- Prozac (fluoxetine): Diarrhea, indigestion, nausea, loss of appetite, dizziness, insomnia, drowsiness
- Zoloft (sertraline): Dizziness, headache, constipation, nausea, indigestion, reduced libido
- Desyrel (trazodone): Constipation, diarrhea, nausea, vomiting, dizziness, backache
Side effects of drugs used to treat anxiety, restlessness, and anger
These medications, which are anxiolytics, are prescribed to agitation, restlessness, and angry behavior that can arise in dementia patients.
- Ativan (lorazepam): Drowsiness, weakness, dizziness, unsteadiness
- Serax (oxazepam): Dizziness, headache, drowsiness, unsteadiness
Side effects of drugs used to treat hallucinations and aggression
These medications, which are antipsychotics, are prescribed to reduce hallucinatory or aggressive episodes.
- Abilify (aripiprazole): Anxiety, constipation, difficulty speaking, loss of balance control, tremor, fatigue
- Clozaril (clozapine): Blurred vision, confusion, constipation, fast heartbeat, nausea, dizziness, tremor
- Geodon (ziprasidone): Headache, anxiety, tremor, constipation, rash, dizziness
- Haldol (haloperidol): Constipation, drowsiness, low blood pressure, uncontrollable restlessness and movements, dry mouth
- Risperdal (risperidone): Aggressive behavior, difficulty speaking or swallowing, loss of balance control, loss of muscle control, and trouble sleeping
- Seroquel (quetiapine): Chills, cold sweats, confusion, dizziness, drowsiness
- Zyprexa (olanzapine): Bloating, body aches, confusion, fever, weight gain, constipation, dizziness
Dealing with side effects
Always report side effects to your doctor. Some side effects are known to be dangerous and may require switching to a new medication. Others are simply bothersome and unpleasant.
Sometimes side effects lessen over time as the body adjusts to the medication. Other times, side effects can be related to non-medication issues—like stomach upset being caused by a spicy dinner rather than a new medication.
If a person experiences side effects, they (or their caregiver) can write them down in the medication list and discuss them at the next doctor’s visit.
Some side effects might be worth accepting if the benefits of the medication outweigh the impact of the side effect. The person with dementia and their caregivers are the ones who get to make that choice.
Preventing and dealing with medication refusal
People living with dementia sometimes forget that they need to take medication and can get agitated when asked to do so. The experts at the Alzheimer’s Association suggest these steps to help prevent medication refusal.
Create a routine around taking medication. In addition to giving medication at the same time every day, establish a routine where the person sits in the same chair, uses the same cup to swallow water, and engages in other repeatable events. Routines may lend a sense of safety and security to prevent medication refusal.
Explain the need for the medication clearly and quickly. People living with dementia can forget what their medication is for or how to take it. No one would want to take medication without knowing why. So make a simple statement before handing over the pill. For example, “This is a pill that will help you sleep better. You take it twice a day. Put it in your mouth, then drink a bit of water.”
If the person refuses to take the medication, try again another time. People with dementia can be agreeable one minute and resistant the next. Someone who refuses medication may be perfectly happy to take it 30 minutes later.
If swallowing becomes a problem, ask their provider or pharmacist if there is a liquid option. Difficulty swallowing can be a problem for people living with dementia, and it can also be a side effect of certain drugs. If a person seems to be physically unable to take their medication, contact their provider right away.
When to get help from the medical team
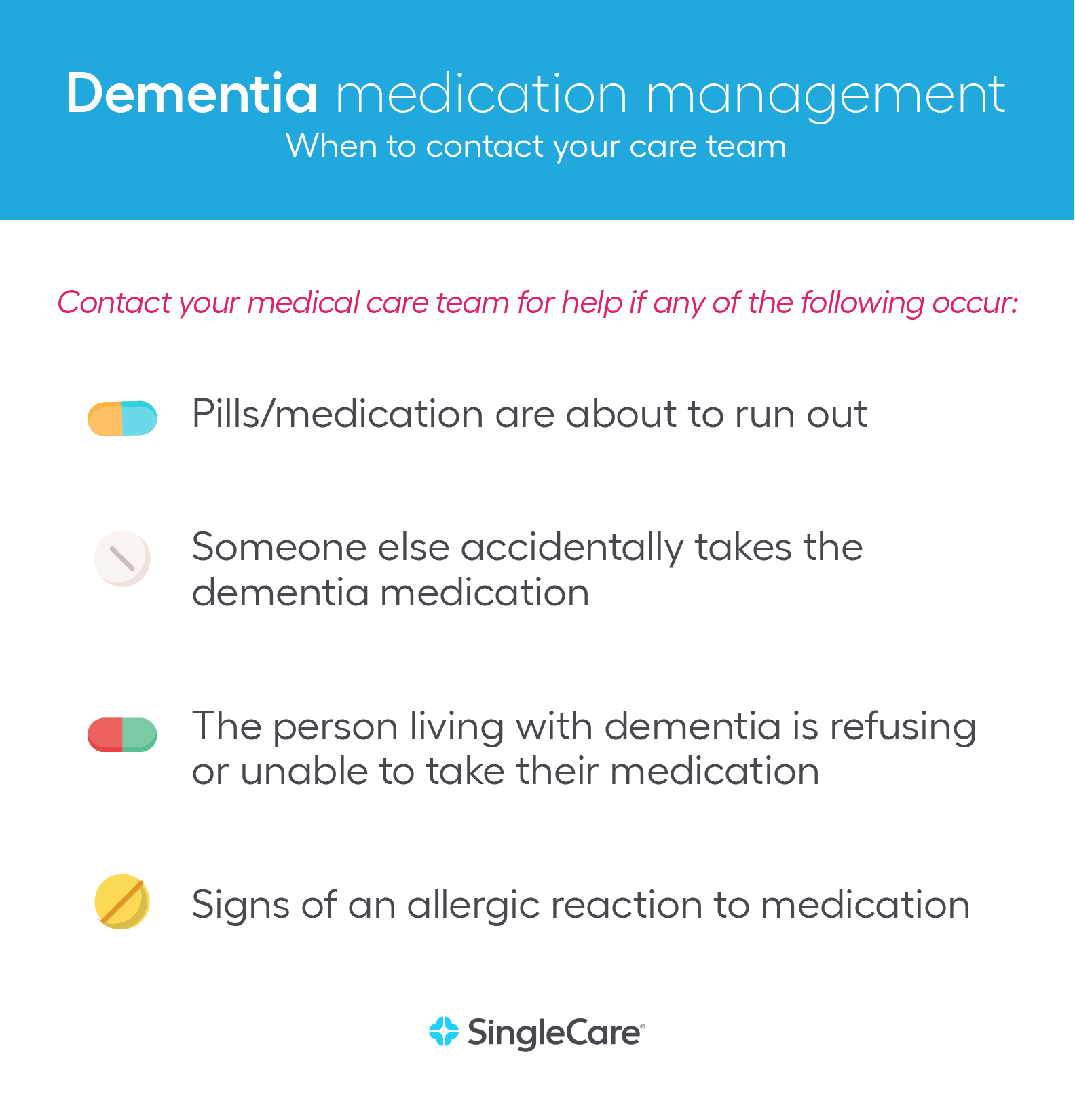
Hopefully, these tips are helpful in creating a safe and successful environment for taking medication at home. But there are times when it’s important to reach out to medical professionals. Here are four situations where you should contact your care team.
- The pills/medication are about to run out: If you find yourself short on pills, act quickly. Call your doctor and pharmacist to see what can be done.
- Someone else accidentally takes the medication: Medication mix-ups do happen. Call your pharmacist or a poison control hotline to see what steps should be taken.
- The person is refusing or unable to take medication/treatment: Whether physical or psychological, problems while taking medication are common. Your care team will have strategies to help.
- Signs of an allergic reaction to medication: Any unusual reaction to medication is something you should contact your care team about immediately.




