Key takeaways
Worldwide, up to 50% of school children are sensitized to common allergens, with allergies being a significant issue in young kids, causing potential severe health consequences.
Allergy testing, which includes skin tests, blood tests, and elimination diets, can identify allergens like plant pollen, foods, and insect stings, aiding in managing symptoms more effectively.
Pediatricians may suggest allergy testing for children with respiratory conditions like asthma or symptoms such as sneezing, coughing, and skin rashes to pinpoint triggers and improve quality of life.
Children of any age can undergo allergy testing, with various tests available depending on the suspected allergies, and costs ranging significantly based on the type of test and healthcare coverage.
Worldwide, the sensitization rate to common allergens among school children is approaching 40% to 50%, according to the World Allergy Organization (WAO). In the United States, 6.5% of children have food allergies, 7.7% of children have hay fever, and 13.5% of children have skin allergies, according to National Health Interview Survey data. The bottom line: Allergies are a common problem for households with young kids.
When allergies are acute, they can have scary health consequences. Kids can lose sleep or miss school after being up all night coughing. Or, in severe cases, have a dangerous reaction to an insect sting or food exposure. Especially with food allergies, it’s important to find the source of symptoms as soon as possible for your child’s safety. “Food is one of the most common causes of anaphylaxis, a rapidly developing and life-threatening allergic reaction, in children, accounting for up to 81% of cases,” says Lakiea Wright, MD, medical director of U.S. clinical affairs at Thermo Fisher Scientific.
If your child has sneezing fits at certain times of year, or develops hives after eating a particular snack—that aren’t controlled by allergy medication—it may be time to consider allergy testing.
The sooner you identify what’s causing symptoms, the sooner you can treat symptoms so your child can go back to regular life.
What is allergy testing?
Allergy testing is a process of skin tests, blood tests, or elimination diet tests that try to pinpoint sensitivity to common allergens such as:
- Plant pollen
- Molds
- Animal dander
- Insect stings
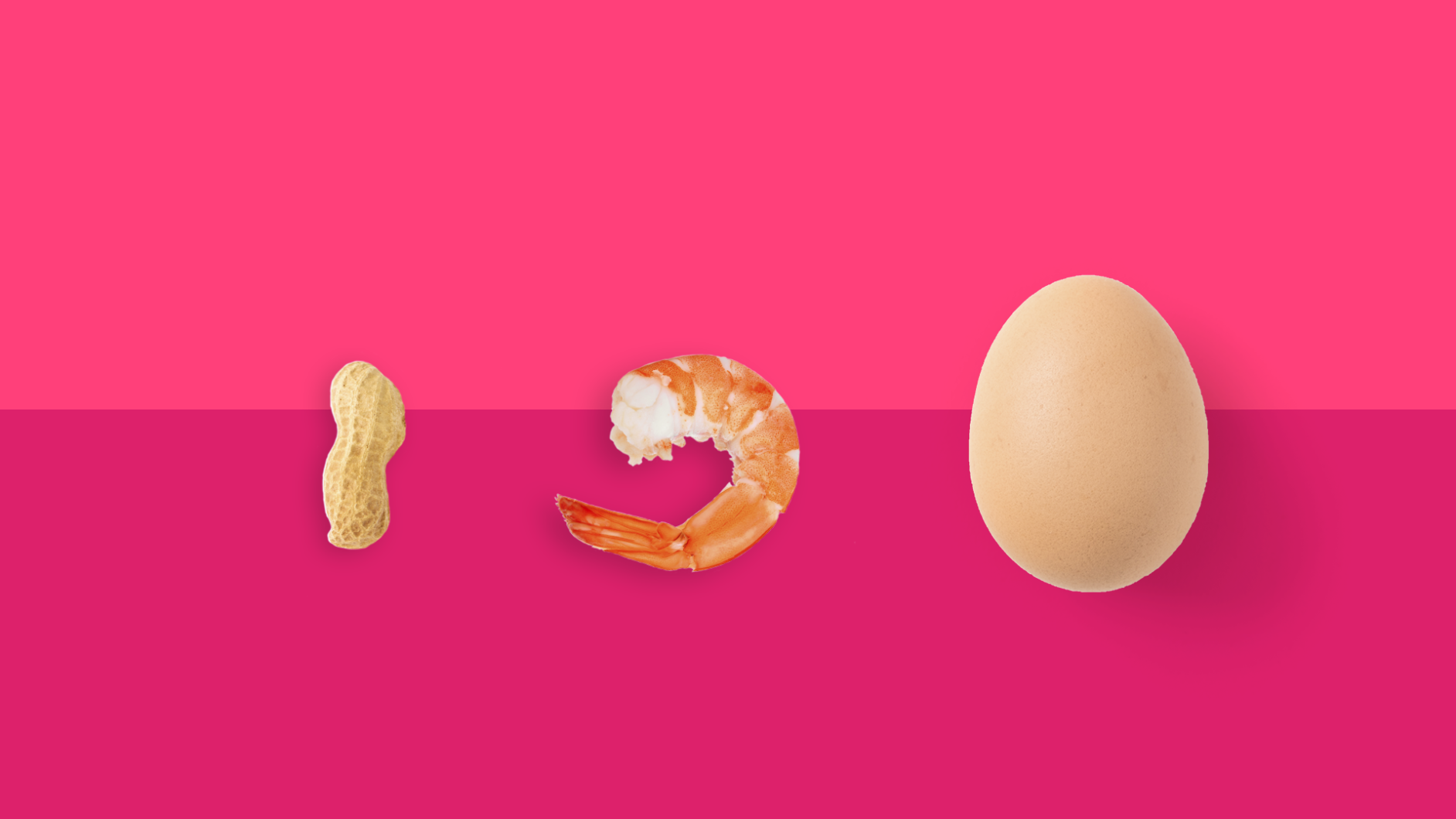
- Foods (e.g., peanuts, eggs, milk, shellfish, or wheat)
- Medications
“These tests can aid in the diagnosis of food allergies and more,” Dr. Wright says. “For example, there is also testing available for common environmental allergies including dust mites, mold, animal dander, and pollens.” The type of testing varies, depending on if your child has environmental or food allergies.
When should parents consider allergy testing kids?
Physicians may recommend allergy testing if your child has a respiratory condition like asthma to find out what triggers symptoms. “Any child with concerns for environmental allergies should undergo allergy testing,” says Gary Soffer, MD, an assistant professor of clinical pediatrics at the Yale School of Medicine. “This helps guide our recommendations for avoidance of triggers, and potentially for immunotherapy in the future.” Common indicators of allergies or an allergic reaction in children include:
- Rhinitis (sneezing, congestion, runny nose, or nasal drip)
- Cough
- Wheezing
- Skin rashes
- Hives
- Itchy eyes or skin
- Digestion problems (cramps, nausea, vomiting, or diarrhea)
Children with environmental allergies, “often present with nasal congestion, itchy eyes, and sneezing,” Dr. Soffer says. “The most concerning symptom, to me, is snoring and mouth breathing because it typically means the child is getting a poor night’s sleep.”
Allergy testing kids can help determine if your child’s symptoms are allergy-related or caused by something else.
However, if you only suspect your child might have a food sensitivity, testing doesn’t always make sense. “Testing for food allergies should never be performed without a clear history of a clinical reaction,” explains Dr. Soffer. “Food panels that are, unfortunately, commonly sent tend to have very high false positive rates and often lead to the unnecessary avoidance of food. It is important to discuss your results with a board-certified allergist who has the resources to perform oral food challenges.”
Who can test a child for allergies?
If your pediatrician thinks your child might have allergies, he or she will likely refer you to see an allergist or immunologist who specializes in allergic reactions and allergy testing.
How old does your child have to be to get an allergy test?
Many parents believe that children must reach a certain age before allergies develop. In actuality, children of any age can have and be tested for allergies according to the American College of Allergy, Asthma, & Immunology (ACAAI).
“A simple blood test can be performed at any age (from infants to the elderly),” Dr. Wright agrees. “When a child has an allergy, it can surface for the first time at any age. Some children stop reacting to certain allergens, such as milk and egg, as they grow, but allergies to foods like nuts tend to remain.”
How do they test kids for allergies?
There are three main types of allergy testing:
- Skin tests
- Blood tests
- Elimination diet tests
Depending on the type of allergy suspected, the allergist will choose the most appropriate allergy test or combination of tests. “The diagnosis of food allergy is complicated,” says Dr. Wright. “In addition to obtaining a detailed clinical history from the patient, many allergists will use a combination of blood and skin testing to confirm a diagnosis.” Here’s what you can expect at your child’s allergy test.
Allergy skin tests
The most common types of skin tests for children are prick or “scratch” tests, intradermal tests, and patch tests. “Skin testing tends to be the most affordable and has the highest predictive value for allergies,” Dr. Soffer says. In a skin prick test, the allergist will tap a small amount of the allergen onto the surface of your child’s skin with a needle. In an intradermal test, the allergist injects a very small amount of the allergen into the top layer of your child’s skin. For patch tests, allergens are applied to adhesive, which are worn on the arm for 48 hours. If your child is allergic, a raised, red bump–that looks and feels like a mosquito bite—will appear.
Typically your child will have a reaction to a prick test or intradermal test within 20 minutes or less, though sometimes redness can appear several hours or up to 48 hours after the allergy test. An allergist will check the reaction to a patch test at set times after the patch is removed. For children with severe allergies, skin tests can sometimes trigger anaphylaxis.
Allergy blood tests
There are many different types of blood tests, depending on the suspected allergen. “Blood testing is often necessary for a multitude of reasons and is an excellent alternative to skin testing,” Dr. Soffer explains.
“A blood test can also help to identify the specific allergenic proteins that trigger food reactions—this type of testing is called allergen component testing,” Dr. Wright says. “For example, if your child has a milk allergy, your health care provider can use your child’s clinical history along with the results of component testing to determine if your child needs to avoid milk in all forms or if your child may be able to tolerate baked milk products like cookies, cakes, or muffins.”
Your child will have blood drawn, and receive allergy test results after a lab processes them—typically in one to two days. Your allergist may recommend blood tests if your child is highly sensitive to allergens because there is no risk of an adverse reaction.
Elimination diet tests
When food allergies are suspected, allergists might recommend a very restricted diet that eliminates certain foods that could be causing an adverse reaction.
The most common food allergens are milk, egg, peanut, tree nuts, wheat, soy, fish, and shellfish, according to FARE. Allergists may recommend elimination diets for a week or longer, and will supervise reactions as foods are removed. If an elimination diet is too difficult to follow, or the allergist suspects your child has outgrown a food allergy, he or she may try a food challenge—giving a small amount of the suspected food in a controlled setting to gauge reaction.
“Once we know what a patient is allergic to the first goal of management is to avoid the things that are causing symptoms,” Dr. Soffer explains. “We work with families on ways to control their child’s environment. If this is not effective, then medication or allergy shots are often necessary.”
It’s scary when you suspect your child might have an allergy, but the sooner you identify what’s really causing symptoms, the sooner you can determine a treatment plan to eliminate them–and get back to normal life.
How much does an allergy test cost?
The cost of allergy testing can range from $60 to thousands of dollars, so it’s important to work with your doctor to choose the right tests for your child. Skin tests range from $60 to $300. Blood tests can cost from $200 to $1,000, according to the ABIM Foundation. Depending on your coverage, health insurance may or may not cover these tests.
Pharmacy discount cards, like SingleCare, can help reduce the price of allergy medications, such as Zyrtec (cetirizine), Allegra (fexofenadine), Claritin (loratadine), or Benadryl (diphenhydramine).